Overview
Irritable bowel syndrome (IBS) is a common long-term recurrent functional gastrointestinal disease that causes persistent abdominal discomfort or pain and bowel disturbances (constipation or diarrhea). IBS has other common names, such as spastic or nervous colon, spastic bowel, and mucous colitis. IBS doesn’t cause severe or life-threatening complications; it also doesn’t increase the risk of other gastrointestinal problems, such as ulcerative colitic or colon cancer. But, it is a very frustrating problem that has a significant impact on the quality of life. Patients with IBS often miss work or school and often need to modify their life and work settings to adapt to this chronic condition. Also, anxiety and depression are common among these patients.
IBS affects about 10-20% of the population. It is common in females. It usually occurs before the age of 45 and becomes less common with age.
IBS symptoms vary from one patient to another, but the most common symptoms are abdominal pain, cramps, constipation, diarrhea, bloating, and urgency to defecate. IBS occurs in flares that usually last for several days then improve or resolve. With gastrointestinal problems, IBS patients may experience sexual or urinary problems. Women may have more symptoms around menstruation time.
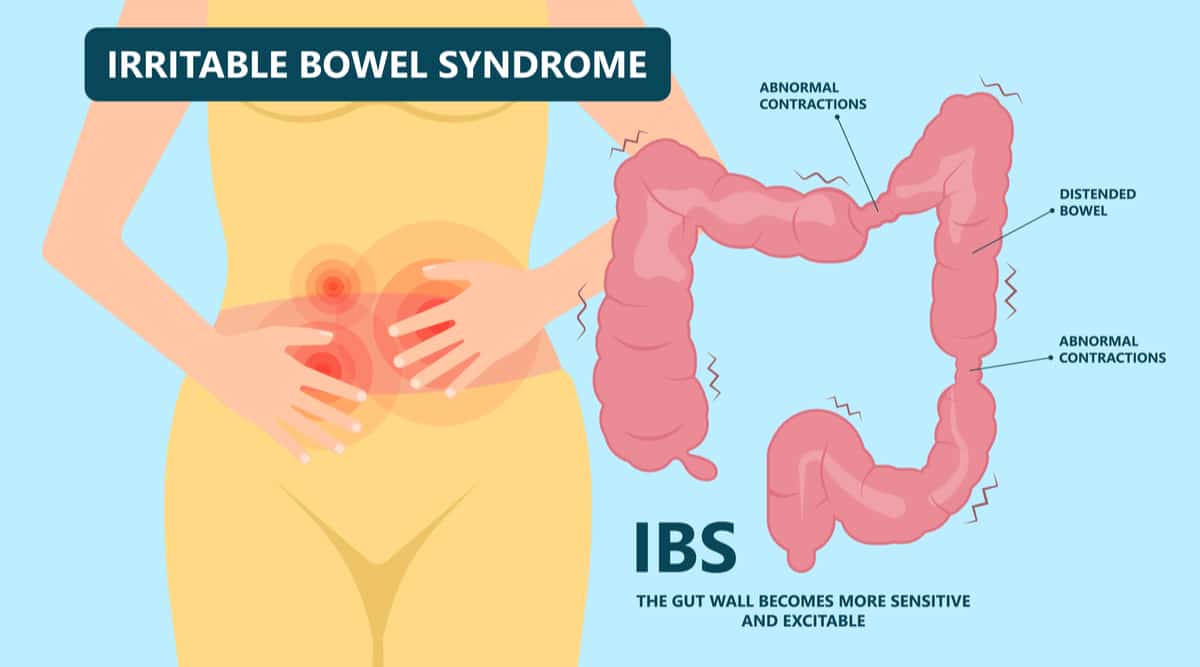
The exact causes of irritable bowel syndrome are unknown. Theories suggest that the colon becomes hypersensitive to mild stimuli, its muscles become spastic, or its movement becomes slow. Other theories suggest that there are disturbances in the body’s chemicals, such as serotonin. Small studies suggested that food poisoning and intestinal infections may be a cause. While the exact cause is unknown, we know several triggers that may be the key to management by avoiding them. These triggers include gastrointestinal infections, psychological stress, and food allergy. Also, there are risk factors, such as young age, female, sex, positive family history, anxiety, and depression.
Read Also:
- Colon Cancer:15 Warning Signs & Symptoms You Should Not Ignore
- Most Common Symptoms, Causes, and Home Remedies Of Stomach Ulcer … Be Aware!
- 8 Foods That Cause Heartburn I What are The Different Foods That Cause Heartburn?
- 10 Pancreatic Cancer Symptoms & Signs Not To Ignore
- 11 Warning Signs Of Gallbladder Cancer You Should Not Ignore!
- Symptoms Of Pancreatitis: 11 Warning Signs Of Pancreatitis
IBS doesn’t have specific laboratory tests or investigations that can diagnose it. The diagnosis depends on the symptoms and exclusion of other serious diseases that may have similar symptoms. The doctor should exclude any worrying features, such as old age, weight loss, rectal bleeding, and anemia. These features may be a red flag for other serious diseases, such as colon cancer, ulcerative colitis, chron disease, coeliac disease, and food intolerance. The investigations depend on what the doctor wants to exclude and may include blood tests, stool examination, abdominal ultrasound, or endoscopy.
The criteria to diagnose IBS (Rome IV criteria) include abdominal pain -for at least one day per week in at least three months-, with two other pain features from the following:
Abdominal pain
- Pain associated with defecation
- Pain associated with a change in the frequency or the appearance of the stool
Irritable bowel syndrome doesn’t have curative treatment. The management plan aims to improve the symptoms and the quality of life. Management plans vary among the patient; no single medication or diet plan works for everyone. The management plans for IBS include diet and lifestyle modifications and medications. The key to managing the symptoms is to know what the triggers are and avoid them. The diet modifications may involve high fiber intake, adequate hydration, a gluten-free diet, and fewer dairy products, cheese, and spicy food. Stress is a significant trigger for IBS that you need to reduce as much as possible; you may need to get more regular exercise, relaxation techniques, or talk therapy.
If the previous measure didn’t control the symptoms, the doctor would prescribe medications to relieve your symptoms. Tell your doctor about any medication that you take to help him to choose the right one. For pain and cramps, antispasmodics, such as dicyclomine, may help. Also, antidepressants help some people with pain and discomfort relief. For constipation, the initial measures are to drink plenty of water and increase the fiber in your diet. But, if there is no adequate response, you will need to use laxatives, such as lactulose, sorbitol, and polyethylene glycol. Also, for constipation, lubiprostone can help. For diarrhea, the first thing is to protect yourself from dehydration. Anti-diarrheal agents, such as loperamide and eluxadoline, slow gut movement and reduces diarrhea. Antibiotics, such as rifaximin, treats bloating and flatulence, and it also treats bacterial overgrowth. Proton pump inhibitors may lead to IBS symptoms; thus, you may need to avoid or stop them. Probiotics and herbal remedies (like peppermint oil) are also helpful.
The cornerstone in irritable bowel syndrome management is patient education. The patient should know what triggers the symptoms and avoid them. Also, the patient should learn how to reduce stress.
In this article, we will discuss -in detail- the following about irritable bowel syndrome:
- What are the symptoms?
- How can we manage it via food?
-
Symptoms of Irritable Bowel syndrome
IBS symptoms occur as an acute attack that usually resolves within one day and usually recurs. The clinical picture of IBS mainly consists of abdominal pain and discomfort, disturbed bowel habits, and abdominal distention.
IBS abdominal pain
is often diffuse all over the abdomen, but its common site is the lower abdomen, especially the left lower quadrant. It usually occurs as cramping, but it may feel like attacks of sharp pain on top of constant dull aching pain. Eating participates, or worse, this pain, and defecation may improve it.
Altered bowel habits in IBS may occur as follows:
Constipation may represent a complaint of hard stools, painful, or infrequent defecation that doesn’t respond well to laxatives.
Diarrhea represents loose stools of small volume, an urgency to defecate, or frequent defecation.
Usually, the patient has one pattern of disturbed bowel habit -constipation or diarrhea-, but some patients may have alternating constipation and diarrhea.
Additional symptoms of IBS
include:
- Mucous in the stool
- Bloating
- Tenesmus: the sense of incomplete evacuation after defecation
- Heartburn and indigestion: gastroesophageal reflux is common among people with IBS
- Headache, nausea, and vomiting
- Food intolerance
- Urinary symptoms, such as frequency and urgency
- Sexual problems: Poor libido or painful intercourse (dyspareunia)
- Psychological symptoms, such as anxiety and depression
- Back pain and frequent fatigue
- Fibromyalgia
In women
In women, IBS symptoms may occur or worsen around menstruation time. After menopause, most women experience fewer symptoms.
The doctor should pay attention to any symptoms inconsistent with IBS because it may indicate organic pathology, and these symptoms include:
- Anorexia and weight loss
- Rectal bleeding
- Old age
- A progressive or acute condition
- Nocturnal symptoms
- Painless diarrhea
- Fever
- Gluten intolerance
- Steatorrhea (fat in the stool)
Irritable bowel syndrome (IBS) types
According to symptoms, we can classify irritable bowel syndrome into four types:
IBS-D; Diarrhea is predominant.
IBS-C; Constipation is predominant.
IBS-M (Mixed IBS); alternating diarrhea and constipation
IBS-U (unclassified); the symptoms don’t fit into any of the above types.
This classification isn’t so important because about 75% of IBS patients change subtypes.
Symptoms of IBS establish the Rome criteria for diagnosis. IBS diagnosis depends mainly on its presentation. To say that it is a case of IBS, we should have the following:
Recurrent abdominal pain at least for one day weekly within the previous three months; the pain also should be:
- Related to defecation (increased or relieved by it)
- Associated with a change (by increase or decrease) in the stool frequency
- Associated with altered stool appearance
The other symptoms are supportive of the diagnosis.
IBS doesn’t cause life-threatening complications or increase the risk of other serious diseases. Its main problem is the chronicity that may affect the patients’ daily activities, such as work or school absenteeism. Some patients need to change their work habits, such as working from home. Also, IBS doesn’t affect life expectancy.
Management of irritable bowel syndrome via diet
Diet represents a common trigger for IBS flares, but also it is a cornerstone of the management plan. IBS symptoms vary from one patient to another; thus, the diet plan should differ according to the patient. The patient should know his/her body. The food and symptoms diary helps the patient to know which food triggers the symptoms. The dietary plan shouldn’t contain only foods to avoid; it should also explain how the patient can get the nutritional value from other sources.
Diet management may take time, but its results are worth the effort. Avoiding the common triggers improves abdominal cramps and bloating and makes bowel movements more regular.
Before we talk about diet modifications, we need to know the most common dietary triggers of IBS, such as:
- Caffeine, coffee, and alcohol
- Dairy products
- High-fat diet
- Sorbitol and fructose (sweeteners)
- Gas-producing foods, such as beans, onions, apricots, and bagels
- FODMAPs (fermentable oligo, di, and monosaccharides and polyols): these foods are difficult to digest, pull water to the intestine, and increase diarrhea and bloating
Now, let’s discuss how the different foods interact with IBS.
Fiber
Generally speaking, fiber is a healthy food that promotes gut health. Food high in fiber includes fruits, vegetables, and whole grains. But, we have two types of fiber: soluble and insoluble fiber. Soluble fibers are present in fruits (like apples and carrots), barries, and oats. Insoluble fibers are present in tomatoes, broccoli, vegetables, nuts, and whole grains.
In IBS, fibers sometimes improve the condition and sometimes worsen it. A high-fiber diet improves constipation, but it also may worsen bloating and diarrhea. Thus, if you have bloating and diarrhea, you should decrease the fibers in your diet. Soluble fibers are a good choice in diarrhea and bloating. If both types worsen the symptoms, you may take soluble fiber supplements, such as psyllium, to get the recommended daily intake (20 to 35 grams daily).
Gluten
Gluten is a protein present in the grains and grain products, such as wheat, rye, barley, bread, pizza, pasta, cakes, and cookies. Some people may be sensitive or intolerant to this protein, and those people may also experience the symptoms of IBS. Avoid gluten for some time, and see if your symptoms improve. If the symptoms improved, you would need to continue on a gluten-free diet.
It is easy to depend on a gluten-free diet because these products become more available every day. You can find gluten-free substitutes for your favorite foods, such as bread, pasta, pizza, cakes, and cookies, in health food and grocery stores. Also, we have nutritious substitutes for gluten-containing grains and flour, such as oats, quinoa, coconut flour, almond flour, and buckwheat.
FODMAP diet
FodMAP diet includes fermentable oligo, di, monosaccharides, and polyols. The intestine can’t digest these carbohydrates easily. Also, these carbs pull water into the intestine, which worsens bloating and diarrhea for IBS patients. You should know that FODMAPs aren’t all carbohydrates; avoid the right foods to get the best results.
These foods include:
- Lactose-containing foods, such as milk, cheese, and yogurt
- Fruits that contain fructose more than glucose, such as apples and pears
- Artificial sweeteners
- Onions, artichokes, broccoli, asparagus, and mushrooms
- Legumes and lentils
- Bread, pasta, cereals that contain wheat
Reduce or avoid these foods for six or eight weeks, and you may experience improvement in your condition. This diet doesn’t mean avoiding all fruits, vegetables, nuts, or dairy products but to choose suitable foods, such as lactose-free milk, soy milk, or rice. Take advice from a dietitian to avoid and eat the right way.
Fatty diet
Generally speaking, a high-fat diet is unhealthy and predisposes to various health problems, such as obesity, hypertension, diabetes mellitus, and heart diseases. A high-fat diet is low in fiber, which is a problem for constipation in IBS patients. A low-fat diet is beneficial for your IBS symptoms and your overall health.
Other foods, such as caffeine-containing drinks, coffee, and chocolate, should be avoided for some time (about 12 weeks) to see if the symptoms will improve.
Limit the alcohol intake as possible because it is a common trigger for IBS symptoms.
What should you avoid, and what should you eat?
Each patient has different triggers; thus, if you are an IBS patient, you should know your body and learn which foods worsen your condition to limit or avoid it.
Diet management should tell you foods to avoid and foods to eat because, if you avoided a food category, you would want to get the nutritional value from another. Thus, talk with your dietitian and physician about your diet plan to get the best possible outcome.
Read Also:
- Colon Cancer:15 Warning Signs & Symptoms You Should Not Ignore
- Most Common Symptoms, Causes, and Home Remedies Of Stomach Ulcer … Be Aware!
- 8 Foods That Cause Heartburn I What are The Different Foods That Cause Heartburn?
- 10 Pancreatic Cancer Symptoms & Signs Not To Ignore
- 11 Warning Signs Of Gallbladder Cancer You Should Not Ignore!
- Symptoms Of Pancreatitis: 11 Warning Signs Of Pancreatitis
Finally, Irritable bowel syndrome is a common but not a dangerous disease (no organic pathology). It only needs you to modify your lifestyle and diet to minimize its impact on your daily life. Follow your doctor’s instructions about lifestyle, diet, and medications, and revise him/her if your condition worsens.