Overview
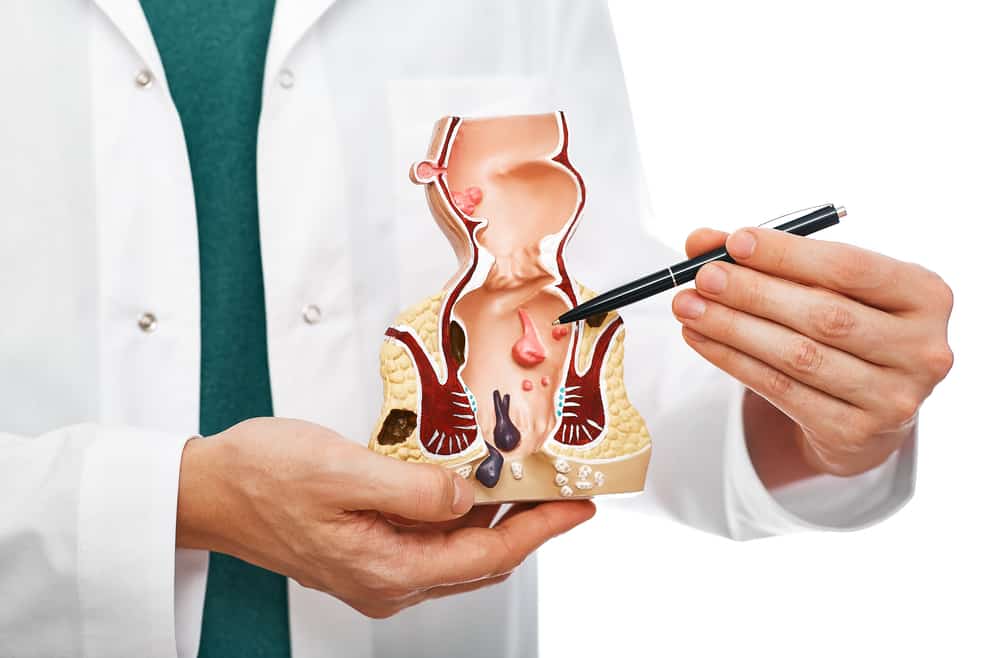
Hemorrhoids (or piles) is a term that describes swollen and bulging blood vessels in the lower rectum and anal canal. Hemorrhoids represent a part of the normal anatomy of the wall of the anal canal that helps in stool control. They become a problem in case of inflammation, swelling, or thrombosis. The term “hemorrhoids” causes some confusion because it describes the normal and pathological state. But here, we will use it for the pathology. According to the site of hemorrhoids, we classify them into two types: internal and external hemorrhoids. The symptoms depend on which type you have. Internal hemorrhoids develop in the lower rectum and often cause painless rectal bleeding. Also, internal hemorrhoids may prolapse and protrude through the anus and cause potential problems, such as itching and pain. On the other hand, external hemorrhoids develop under the anal skin and irritate it, which results in an uncomfortable condition. Also, external hemorrhoids are susceptible to thrombosis, which causes acute and severe painful swelling.
Hemorrhoids are one of the most common causes of anal complaints. About 50% to 65% of the population experience some of the symptoms of hemorrhoids at some point in their lives. The risk of hemorrhoids increases with age and peaks between 45 and 65 years, but external hemorrhoids are common among middle-aged adults. It affects both sexes at an equal rate (no sex prediction), but the pregnancy may increase the risk.
The exact cause of hemorrhoid is unknown, but some risk factors predispose to the condition, such as a low-fiber diet, straining, and constipation.
Read Also:
- Colon Cancer:15 Warning Signs & Symptoms You Should Not Ignore
- Breast Cancer I 14 Treatment For Breast Cancer
- 10 Pancreatic Cancer Symptoms & Signs Not To Ignore
- 11 Warning Signs Of Gallbladder Cancer You Should Not Ignore!
- 8 Warning Signs Of Prostate Cancer I Prostate Cancer Symptoms
- Lung Cancer Symptoms I 10 Warning Signs Of Lung Cancer You Should Not Ignore
A simple history and physical examination can diagnose hemorrhoids. But your doctor may need to exclude other more serious diseases (like colon cancer and ulcerative colitis), especially in the case of rectal bleeding. To confirm the diagnosis and rule out the other conditions, your doctor may do a colonoscopy.
Hemorrhoids don’t require treatment if they are asymptomatic. Management includes conservative management, minor procedures, and surgery. The initial measures, such as adequate hydration and high fiber intake, improve the condition. Analgesics may help in pain relief, and some topical creams may decrease the itching. If the conservative management failed to control the symptoms, the doctor would do some minor procedures -at the office- to shrink or remove the hemorrhoids. Surgery becomes an option after the failure of the other measures. The best treatment for hemorrhoids is prevention by diet and lifestyle modification.
Generally, most cases resolve without treatment or with conservative treatment alone, but some complications may occur, such as infection, ulceration, and thrombosis.
In this article, we will answer -in detail- the following questions about hemorrhoids:
- What are the symptoms and types of hemorrhoids?
- What are the causes and risk factors of hemorrhoids?
- How can doctors diagnose this condition and confirm their diagnosis?
- When do these patients need treatment? And, what are the treatment options for hemorrhoids?
-
Symptoms and types
Most cases of hemorrhoids are asymptomatic. The most often symptoms are:
- Painless bleeding
- Anal pain and itching
- Painful defecation
- Itchy or painful swelling around the anus
Each patient show symptoms according to the type of hemorrhoids that he/she has. Hemorrhoids are external or internal, and each of these types shows a different presentation.
-
External Hemorrhoids
External hemorrhoids exist under the skin of the anus, which has rich innervation by pain fibers. The main problem of external hemorrhoids is when they become thrombosed. Thrombosis causes stretch of the anal skin and surrounding edema, which causes sudden severe pain and hard swelling around the anus. On rare occasions, thrombosed hemorrhoids may invade the skin and bleed. Also, external hemorrhoids cause perianal itching.
The pain resolves within a week, and the swelling may take a few weeks. But the stretched anal skin may persist as a skin tag or redundant skin. This redundant skin can cause hygiene issues.
Without excision of the hemorrhoids, treating thrombus doesn’t prevent the pain recurrence, which reaches the rate of 40%.
-
Internal hemorrhoids
Internal hemorrhoids are present in the lower rectum, and this area has no cutaneous nerves that transmit pain; thus, it is usually a painless condition. The inflamed and swollen hemorrhoids have a thin wall, and the passage of hard stool against the hemorrhoids cause bleeding during or after defecation. Inflamed hemorrhoids also secrete mucous that irritates the skin around the anus and causes itching and burning sensation. Internal hemorrhoid may be painful when:
- They become thrombosed or necrosed.
- They prolapse through the rectum and anus, which causes muscle spasms in this area.
- Internal hemorrhoids have four grades:
Grade 1: Just prominent hemorrhoids without prolapse
Grade 2: Prolapse occurs during straining with spontaneous reduction
Grade 3: Prolapse occurs during straining but requires manual reduction
Grade 4: Prolapsed hemorrhoids and the manual reduction can’t reduce it
Hemorrhoids aren’t a dangerous condition; life-threatening bleeding -or even bleeding that causes anemia- is rare. But, symptoms, such as rectal bleeding or perianal itching, and pain, require ruling out other more concerning causes.
Differential diagnosis of hemorrhoids
- Fissures
- Abscesses
- Fistulas
- Colorectal cancer
- Inflammatory bowel diseases: Ulcerative colitis and chron’s disease
- Genital warts
- Acute proctitis
- pruritus ani
- Anorectal varices of portal hypertension
-
Causes and risk factors of hemorrhoids
The exact causes of hemorrhoids are unknown. Hemorrhoids are a part of the natural human anatomy, but they become a problem when they swell. This swelling may occur due to increased pressure on the hemorrhoidal vessels. The following risk factors may predispose to the condition:
- Prolonged straining
- Bowel disturbances, either constipation or diarrhea
- Diet with low fiber content causes small-sized stools, which causes more straining during defecation.
- Pregnancy; Enlarged uterus increases the pressure on the hemorrhoid vessels and causes or increases their swelling. Also, during pregnancy, the hormonal changes may weaken the supportive muscles of the rectum and anus.
- Ascites and intra-abdominal mass
- Prolonged sitting on the toilet
- Chronic cough
- Obesity and lack of physical activity
- Lack of erect position
- Spinal cord injuries
- Previous rectal or anal surgery
- Colon cancer
- Aging and positive family history
- Genetic predisposition, such as the presence of hemorrhoidal veins without valves
- Anal sex
- Repeated lifting of heavy objects
All of the previous factors may cause or worsen hemorrhoids.
-
Diagnosis of hemorrhoids
The diagnosis of hemorrhoids starts with the history. Most doctors blame the hemorrhoids for all anorectal complaints. A good doctor should take a careful history to detect the problem source and narrow the differential diagnosis before the examination. The most common presentations of hemorrhoids are rectal bleeding, perianal itching, and pain, which are nonspecific symptoms that occur with other serious diseases. Thus, the doctor should depend on a good history and physical examination to confirm the diagnosis. Also, the doctor should ask about the risk factor, such as diet, family history, prolonged straining, and heavy lifting.
After the history, the doctor will do a physical examination that includes visual inspection, digital rectal examination, and endoscopies (if possible and appropriate). Visual inspection of the anus can detect external hemorrhoids or prolapsed internal hemorrhoids. By visual inspection, the doctor can see:
- Skin tags (redundant skin)
- Prolapsed hemorrhoids
- Abscesses, fissures, or fistulas
The digital rectal examination enables the doctor to feel abnormal structures, such as masses. This examination may be uncomfortable for the patient if there is severe pain or spasm. Also, digital rectal examination can’t feel the internal hemorrhoids. In this examination, the doctor puts a gloved, lubricated finger through the rectum. The patient should be in the left lateral position with flexed knee towards the chest. Topical anesthetics may be useful to relieve any discomfort during the examination.
Visual inspection and digital examination can’t detect internal hemorrhoids. Thus, the doctor will do an anoscopy to look through the anal canal. Anoscopy is an office procedure where the doctor uses a short, plastic, and lighted tube to look through the anus.
If the symptoms are still confusing, such as rectal bleeding, and the doctor wants to exclude other serious causes, he can do the following:
- Sigmoidoscopy:
The doctor uses a flexible-lighted tube (sigmoidoscope) to look into the lower part (the last 40 cm) of the colon (sigmoid colon).
- Colonoscopy:
The doctor uses a flexible-lighted tube to look through the entire colon.
After the previous history and examination, the doctor can decide if the patient has hemorrhoids or the complaint is due to another cause; thus, the doctor can start the appropriate management plan.
-
Management of hemorrhoids
The management plan of hemorrhoids depends on the type and the severity of the condition. Hemorrhoids only need treatment when they become symptomatic and bother the patient. Asymptomatic hemorrhoids don’t need treatment they look bad to the doctor. According to the case, there are three options for the management of hemorrhoids:
- Conservative Management
- Office-based Procedures
- Surgery
- Conservative management is the first-line management for non-thrombosed external and grade 1 internal hemorrhoids. This management option aims to control the symptoms of hemorrhoids, not their appearance. Conservative treatment includes the following measures:
- High-fiber diet
Increased fiber intake cures constipation and straining and may relieve the symptoms, such as bleeding and pain, only without other treatment. You can raise your fiber consumption by diet modification or fiber supplements, such as methylcellulose and psyllium seed.
- Warm baths-for 10 to 15 minutes several times per day- relieve the pain of hemorrhoids. Warm water relaxes the muscle spasm that causes the pain.
- Ice packs can relieve the pain and swelling of acute thrombosis.
- Toilet habits modification
The patient should reduce the time of sitting on the toilet; it’s enough to sit only to evacuate the lower intestine without straining as possible. Prolonged sitting increases the straining and worsens the symptoms.
- Prevention of constipation and diarrhea
Anti-diarrheal agents and stool softeners may help. Also, high fiber intake prevents bowel disturbances.
Medications
Medical treatment in hemorrhoids aims to relieve the pain, inflammation (itching), and any bowel disturbances (constipation or diarrhea).
Topical anesthetics, such as lidocaine ointment 5%, help in pain control. Analgesics, such as paracetamol, also help in pain relief.
Mild astringents, such as witch hazel, relieve the itching.
Topical steroids also may help in itching relief. But, it is used only for a limited period due to its side effects.
- Conservative therapy may lead to complete resolution in many patients.
- Office-based non-surgical procedures
When the conservative therapy can’t control the symptoms, the doctor will do a non-surgical procedure to destroy the hemorrhoids. This option is the best for grades one, two, and three internal hemorrhoids. These procedures are safe, and their side effects are so rare. These procedures include:
Rubber band ligation
It is the best and the most commonly used procedure. In this procedure, the doctor applies a band to the hemorrhoid to cut off its blood supply. Banded hemorrhoid falls off within one week, leaving a scar. For complete treatment, the doctor may need to repeat this procedure.
Sclerotherapy
The doctor injects a sclerosing agent (like phenol) into the hemorrhoids. The vein of injected hemorrhoid collapses, and this hemorrhoid falls.
Other procedures are available, such as electrocautery, laser therapy, and infrared radiation. Your doctor will discuss with you which is the best for you.
-
Surgery (Hemorrhoidectomy)
If the conservative therapy and medical procedures failed to control the condition, surgery would be the choice. As with all surgeries, hemorrhoidectomy (surgical excision of hemorrhoids) may have some complications, such as postoperative pain, bleeding, infections, and urine retention. Hemorrhoidectomy is the best choice for:
- Thrombosed external hemorrhoids within 72 hours of the symptoms
- Grade three and four internal hemorrhoids with severe symptoms
- Associated problems, such as hygiene problems due to skin tags
Hemorrhoidectomy requires general anesthesia, but the patient can go home within a day and return to work within ten days. After the surgery, the patients should have long-term monitoring till complete healing occurs. Also, the patients should avoid constipation, straining, prolonged sitting on the toilet, and improve their anorectal hygiene.
Other surgical options include:
Stapled hemorrhoidectomy
The surgeon removes the prolapsed hemorrhoidal tissue and returns the hemorrhoids to their position. It is less painful and faster than traditional hemorrhoidectomy but with a higher recurrence rate.
Prevention
The following measures will help in the prevention of hemorrhoids:
- High fiber intake
- Keep a healthy weight.
- Exercise
- Maintain adequate hydration
- Modify your bowel habits, such as avoiding straining, constipation, and prolonged sitting on the toilet
These measures and those of conservative therapy can prevent hemorrhoids and control mild cases.
Read Also:
- Colon Cancer:15 Warning Signs & Symptoms You Should Not Ignore
- Breast Cancer I 14 Treatment For Breast Cancer
- 10 Pancreatic Cancer Symptoms & Signs Not To Ignore
- 11 Warning Signs Of Gallbladder Cancer You Should Not Ignore!
- 8 Warning Signs Of Prostate Cancer I Prostate Cancer Symptoms
- Lung Cancer Symptoms I 10 Warning Signs Of Lung Cancer You Should Not Ignore
Finally, hemorrhoids are benign conditions, that only require treatment when they represent a problem, and their treatment is available and highly successful.
Before we say the hemorrhoids are the problem, we should exclude the other dangerous conditions that may have similar symptoms.