Lymphedema is characterized by the accumulation of lymphatic fluid in tissues, leading to swelling and inflammation. It typically occurs when the lymphatic system – draining excess fluid and waste products from the body’s tissues – is impaired or damaged. Lymphedema commonly affects the arms and legs but can also develop in other body parts. There are two main types of lymphedema:
- Primary Lymphedema:This type usually occurs at birth or develops later in life due to a congenital abnormality or genetic predisposition. It can manifest at various ages and may become apparent in adolescence or adulthood.
- Secondary Lymphedema:Secondary lymphedema is more common and typically occurs due to damage to the lymphatic system. Common causes include surgical procedures (such as lymph node removal during cancer surgery), radiation therapy, infection, trauma, or other medical conditions that affect lymphatic flow.
Lymphedema can present with various symptoms, and it’s essential to recognize these warning signs to seek early diagnosis and treatment. Here are 12 lymphedema symptoms you should be aware of:
1. Swelling
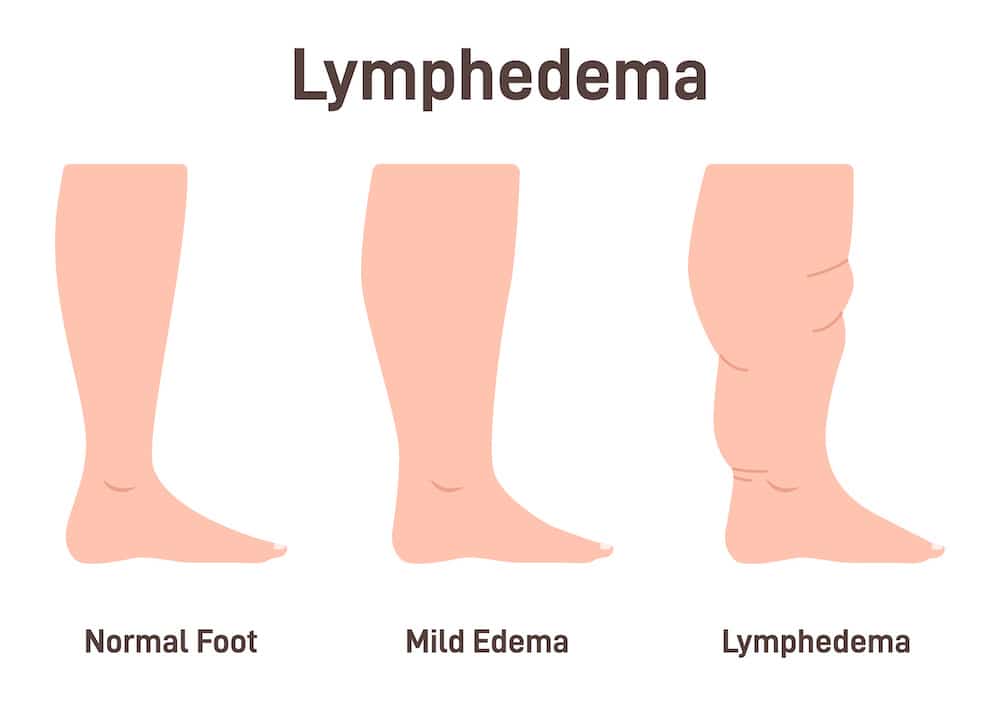
Lymphedema leads to the abnormal buildup of lymphatic fluid in the tissues, which causes the affected limb or area to become visibly swollen. This swelling can vary in severity and may start gradually or suddenly, depending on the cause and individual factors.
Swelling is usually the most noticeable and concerning symptom of lymphedema, prompting individuals to seek medical attention. It’s important to remember that lymphedema is a chronic condition, and early detection and management can help control the swelling and prevent complications.
2. Pitting edema
Pitting edema occurs because the excess lymphatic fluid is not draining properly from the affected area. This fluid buildup creates increased pressure within the tissues, causing them to become more compressible. When pressure is applied, it displaces the excess fluid, resulting in a temporary pit. However, because the lymphatic system is compromised, the fluid returns to the area relatively quickly once the pressure is released.
The presence of pitting edema is an important diagnostic feature for healthcare professionals when evaluating the possibility of lymphedema. The depth and duration of pitting can help determine the severity of the condition. Healthcare providers use this information to plan appropriate treatment strategies and monitor progress.
3. Restricted range of motion
Lymphedema can reduce the ability to move the affected limb or joint due to the swelling and pressure on surrounding tissues. This symptom is often a result of the buildup of excess lymphatic fluid and the subsequent tissue fibrosis (thickening and hardening) that can occur in the advanced stages of the condition.
4. Heaviness and tightness
In lymphedema, heaviness and tightness refers to the feeling of increased weight or pressure in the affected limb or area. It may feel as though the limb is heavier than usual. This sensation arises because of the accumulation of excess lymphatic fluid and swelling in the tissues. As fluid builds up, it puts pressure on the surrounding tissues, leading to the perception of heaviness. This can make the affected limb or area feel more cumbersome and can interfere with everyday activities and movements.
5. Skin Changes
Lymphedema can bring about various skin changes in the affected area, often indicative of the chronic swelling and fluid accumulation associated with the condition. Over time, the skin in the affected area may become thicker and firmer due to the buildup of lymphatic fluid and proteins in the tissues. This thickening is known as fibrosis. In addition to thickening, the skin may harden or feel firm to the touch. This results from the increased tissue density caused by fluid accumulation and cellular debris.
6. Achy or Painful Sensations
Some individuals with lymphedema may experience discomfort, aching, or pain in the affected area. This pain or achiness can vary in intensity and may be constant or intermittent. The sensations are often related to the increased pressure and swelling in the affected tissues.
Lymphedema causes a buildup of lymphatic fluid in the tissues, leading to swelling and increased pressure on surrounding structures like blood vessels and nerves. This pressure can result in discomfort and pain. The chronic inflammation associated with lymphedema can contribute to pain and discomfort. As the tissues become more inflamed, the sensations of achiness or pain may intensify.
7. Clothing and Jewelry Tightness
Lymphedema causes an increase in the size of the affected limb or area. As a result, clothing, like sleeves, pants, or even shoes, that previously fit comfortably may feel tight or constricting when worn over the swollen body part.
This symptom can be particularly noticeable because it can affect a person’s day-to-day comfort and ability to wear their regular clothing and accessories. It is a practical indicator of the swelling associated with lymphedema and can be a sign for individuals to seek medical evaluation and treatment. Managing lymphedema typically involves wearing compression garments or using bandages to reduce swelling and improve comfort, allowing individuals to wear their regular clothing more comfortably.
8. Elevation may help
Raising or elevating the affected limb or area can temporarily relieve some of the discomfort and swelling associated with lymphedema. When you elevate the affected limb or area, you essentially use gravity to assist the lymphatic system in draining excess fluid and waste products away from the swollen area. This can help reduce swelling, improve circulation, and alleviate some of the pressure and discomfort associated with lymphedema.
9. Delayed Wound Healing
Delayed wound healing is when wounds, injuries, or skin abrasions in the affected area take longer to heal compared to wounds on unaffected parts of the body. This symptom indicates the compromised lymphatic system’s ability to support the body’s natural healing processes.
Lymphedema, whether primary or secondary, is characterized by a disruption in the normal flow of lymphatic fluid, which contains immune cells and plays a crucial role in maintaining tissue health and fighting infections. When the lymphatic system is compromised, as is the case in lymphedema, the removal of excess fluid, waste products, and immune responses from the affected area becomes less efficient.
Wound healing involves inflammation, cell proliferation, tissue remodeling, and immune responses. When the lymphatic system is impaired, it can lead to prolonged inflammation and fluid buildup at the site of a wound, making it harder for the body to clear away debris, deliver nutrients, and support the repair process.
10. Increased Risk of Infections
Individuals with lymphedema are at an increased risk of developing infections in the affected area. This increased susceptibility to infections is primarily due to the compromised lymphatic system’s reduced ability to clear away bacteria, foreign particles, and waste products from the tissues, making it easier for infections to take hold.
Lymphatic fluid is crucial in carrying immune cells throughout the body to help fight off infections. In lymphedema, the stagnation of lymphatic fluid can result in decreased immune function in the affected area, making it harder for the body to defend against invading pathogens.
Plus – the accumulation of lymphatic fluid can limit the delivery of oxygen, minerals, and essential nutrients to tissues in the affected area. This can weaken the body’s ability to repair and regenerate damaged tissue and fight infections effectively.
11. Enlarged Lymph Nodes
There can be some situations in which lymph nodes become enlarged in the context of lymphedema:
- Infection: Infection is a concern for individuals with lymphedema because the compromised lymphatic system may not be as effective at fighting off infections. In response to an infection in the affected limb or area, nearby lymph nodes may become enlarged as they work to filter and process the infection.
- Cellulitis is a skin infection (usually caused by bacteria) that can occur in people with lymphedema, particularly in the affected limb. When cellulitis develops, it can cause inflammation and enlargement of regional lymph nodes as the body’s immune system responds to the infection.
- Inflammatory Reactions: In some cases, the swelling and changes in tissue associated with lymphedema can trigger inflammatory responses in the body, potentially leading to the enlargement of nearby lymph nodes. Furthermore, it may lead to lymphadenitis – an inflammatory condition of the lymph nodes. It also worsens the outcome and trigger various complications.
Take away
Lymphedema is a chronic accumulation of lymphatic fluid in tissues, resulting in swelling and various symptoms. It can occur in different body parts and is classified into primary and secondary lymphedema. Recognizing early signs of lymphedema is crucial. These signs include swelling, a feeling of heaviness or tightness, restricted range of motion, pitting edema, skin changes, recurrent infections, and more. Recognizing long-term effects of lymphadenitis on various body organs is also equally important to prevent complications and improve prognosis (outcome).
It is also triggered by several factors such as food, stress, trauma, and other medical conditions. Certain foods and medications are known to trigger and exacerbate the retention of water and sodium in the body – means increase in the severity of lymphedema. Early diagnosis and tailored intervention are critical in preventing complications and managing lymphedema effectively. If you suspect you have lymphedema or are at risk, consult a healthcare professional for evaluation and personalized treatment.