Overview
Ulcerative colitis is one of the two pictures of inflammatory bowel disease; the other picture is Crohn’s disease. It is a chronic inflammatory disease that destroys the lining of the colon and rectum and causes ulcers. It doesn’t only affect the gastrointestinal tract, but also it can affect the skin, bone, joints, and eyes. Ulcerative colitis may lead to severe and life-threatening complications. But, proper management can control the condition, relieves its social and emotional impact, and reduce the risk of long-term complications. Ulcerative colitis develops gradually over a long time. Its course is intermittent, which means that it consists of flares and remissions.
Ulcerative colitis is more common than Crohn’s disease by three times. It is more common in the western populations, such as Europe and North America; it affects about one million people in the united states. Each year, it affects about 10 to 20 new patients per 100,000 people, and about 50 to 500 patients already have the disease. Ulcerative colitis affects all ages, but it has two age peaks. It is common among people between 15 and 25 years and those over 55 years. It affects males and females at an equal rate.
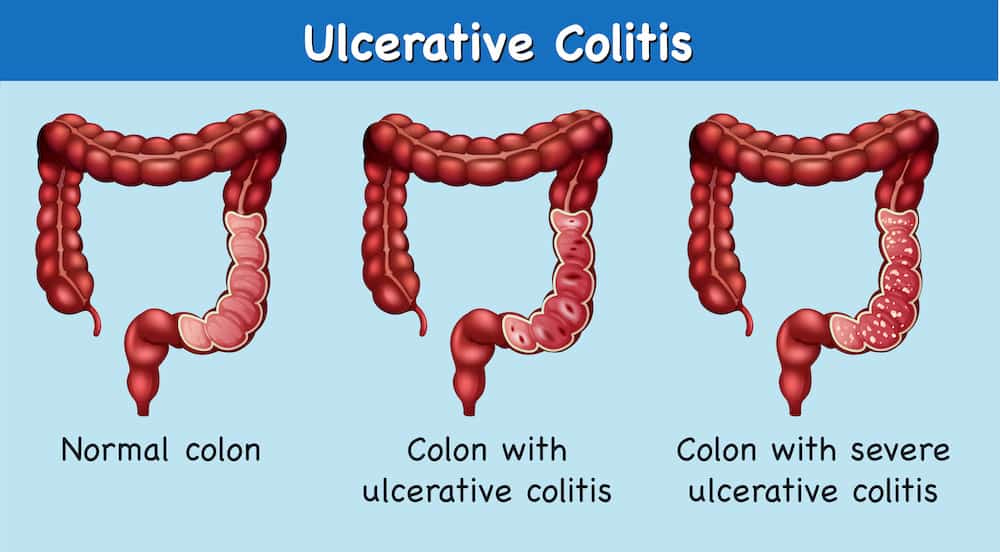
Symptoms of ulcerative colitis occur in attacks and vary according to the severity and site of the inflammation. The main symptoms are abdominal pain, bloody diarrhea, tenesmus, and rectal bleeding. It also may cause anemia, fatigue, fever, and weight loss. It is uncommon for children, but if it occurred, it would cause growth retardation. Besides the gastrointestinal symptoms, there are extraintestinal symptoms, such as eye pain (uveitis), painful and swollen joints (arthritis), osteoporosis, and skin manifestation (ulcers or nodules). Ulcerative colitis also raises the risk of colon cancer. Other diseases may occur with ulcerative colitis, especially liver diseases (called primary sclerosing cholangitis). According to the severity, ulcerative colitis may be mild, moderate, or severe; most patients experience mild to moderate symptoms. Also, ulcerative colitis has another classification according to its site, rectum, part of the colon, or the whole colon.
Ulcerative colitis has no clear causes, but some risk factors may contribute to the disease or aggravate its symptoms. Some hypotheses suggested that genetic predisposition, immune system malfunction, and environmental factors may play a role. Other aggravating and risk factors include:
Risk factors
- Age
- Race: The risk is higher among whites and Ashkenazi Jewish.
- Positive family history
- Vitamins A and E (antioxidants) deficiency
- Psychological stress
- Milk consumption
The smoking effect on ulcerative colitis is unusual. Unlike Crohn’s disease, ulcerative colitis is less common among smokers. Also, there is some evidence about the protective role of smoking in ulcerative colitis.
Diagnosis of ulcerative colitis should exclude other diseases that show similar symptoms, such as Crohn’s disease and colon cancer. Doctors have many investigations that can diagnose ulcerative colitis, exclude other conditions, and evaluate the patient’s status. Endoscopic techniques and tissue biopsies make the definitive diagnosis. Endoscopic procedures show the ulcers and determine their site. We have other tests and investigations to help the doctor to see if you have dangerous complications. Blood tests check for anemia that may occur due to rectal bleeding. Stool examination detects gut infections that have symptoms similar to ulcerative colitis. Stool examination also detects other specific proteins (calprotectin). Also, your doctor may order other serological tests to look for specific antibodies. Other tests may include barium enema, CRP, and ESR. Your doctor may need imaging techniques, such as X-ray, CT scans, and ultrasound, if the symptoms suggest serious complications, such as a perforated colon.
Ulcerative colitis has no curative medical treatment. The management plan depends on the severity of the condition and aims to relieve the symptoms as possible, help the colon heal, and reduce the frequency of attacks. The management plan involves three lines: diet modifications, medications, and surgery.
Each patient may experience worsening with some foods different from the other patients. Thus, there is no specific diet for all patients; each patient should avoid any food that worsens his/her condition. Medical treatment aims to fight the symptoms, induce remission, and maintain it. Medications include:
- Anti-inflammatory drugs, such as aminosalicylates and steroids
- Immunosuppressors, such as azathioprine and cyclosporine
- Biologics, such as infliximab
- Other medications, such as antidiarrheal drugs, antispasmodics, and analgesics
The choice of medications depends on your symptoms, type, and severity of the disease. Thus, talk with your doctor before taking or stopping any medication.
If the previous options didn’t control the disease or give the desired outcome, surgery would be the choice. Surgery may remove the entire colon and rectum, which cures ulcerative colitis, but it has risks and impacts on your life that your doctor should discuss with you. Surgery may be urgent or elective.
In this article, we will answer -in detail- the following questions about ulcerative colitis:
- What is the clinical picture of ulcerative colitis?
- What are the effective treatment options that can control this disease and improve the quality of life?
The clinical picture of ulcerative colitis
Ulcerative colitis causes a general inflammatory status that causes intestinal and extraintestinal symptoms. Symptoms occur in attacks with periods of remission in between. Symptoms vary among patients according to the severity and the site of inflammation.
1. Intestinal symptoms
The main symptom of this disease is the frequent bloody diarrhea that may contain mucous or pus. Abdominal pain also occurs and may be mild discomfort or so painful bowel movements and abdominal cramps. Bloody diarrhea and abdominal pain are the characteristic features of severe attacks.
Other symptoms include:
- Frequent urgency to defecate
- Fecal incontinence
- Nocturnal defecation
- Tenesmus: urgency to defecate but without passage of stool (or too little stool)
- Chronic rectal bleeding is a dangerous problem that may cause anemia, which affects the quality of life.
- Rectal pain
- Fever, fatigue, malnutrition, weight loss, iron deficiency
- In children, ulcerative colitis causes growth retardation.
Ulcerative colitis causes life-threatening complications, such as:
- Perforated colon
- Toxic megacolon (rapidly dilated colon)
- Severe dehydration
- Severe anemia
- Raised risk of colon cancer
Intestinal symptoms classify ulcerative colitis into three grades:
- Mild: Rectal bleeding and less than four bowel motions daily
- Moderate: Rectal bleeding and more than four bowel motions daily
- Severe: Like the previous grade plus systemic (extraintestinal) symptoms and low serum albumin (due to dehydration)
2. Extraintestinal symptoms
The inflammation of ulcerative colitis extends to affect organs other than the colon, such as skin, eyes, bone, joints, and liver.
- The mouth is on the affected areas. Mouth lesions occur as mouth ulcers, such as in aphthous stomatitis or angular cheilitis. Aphthous stomatitis is recurrent and benign mouth ulcer. Angular cheilitis is painful ulcers at the mouth angle that may extend to the skin.
- Skin manifestations also occur and include erythema nodosum and pyoderma gangrenosum. Erythema nodosum is the most common skin problem and indicates disease activity. It consists of elevated, tender, and red nodules, usually on the shins. Pyoderma gangrenosum is a more severe lesion; it consists of painful nodules and pustules (pus-filled vesicles) that may ulcerate.
- The eye is also one of the affected organs, especially the iris causing its inflammation (iritis). Eye symptoms include photophobia (eye pain on light exposure) and blurred vision. Iritis requires rapid and proper treatment to avoid permanent vision loss. Eye inflammation may also involve the sclera and episclera.
- Ulcerative colitis can also involve the joints and cause arthritis, which causes painful, red, hot, tender, and swollen joints with limited movement. It has a significant impact on daily life quality. It may involve large joints, such as hip and shoulder joints, or small joints of the hands and feet. It also affects bone and causes osteoporosis, which raises the risk of bone fractures.
- Patients with ulcerative colitis have an increased risk of blood clots by three times more than others. Blood clots manifest as painful leg swelling in deep venous thrombosis or difficult breathing in pulmonary embolism.
- Anemia may occur in ulcerative colitis due to chronic blood loss. Also, it may occur due to bone marrow depression as a result of the chronic disease or due to autoimmune destruction of the red blood cells (autoimmune hemolytic anemia).
- The liver is also one of the affected organs in ulcerative colitis. 5% of patients with ulcerative colitis have primary sclerosing cholangitis (PSC). It is an inflammatory disease that destroys the small and large bile ducts. 75% of the patients with primary sclerosing cholangitis have ulcerative colitis. PSC leads to obstructive jaundice and may end in liver cell failure and liver cirrhosis. It also increases the risk of bile duct cancer and colon cancer. There is no specific curative treatment for PSC. Also, colectomy doesn’t relieve it. Despite the association, the courses of ulcerative colitis and PSC are unrelated.
See your doctor if you have any of the prominent intestinal symptoms to discover ulcerative colitis early if it presents. Early diagnosis helps the management plan to be more effective. It also gives the doctor a chance to prevent life-threatening complications and reduce the disease’s impact on your daily life.
Management of ulcerative colitis
There is no curative treatment for ulcerative colitis except the surgical removal of the colon, and this surgery has a significant impact on the patient’s life. Medical treatment is the initial measure in the management plan, and it aims to induce and maintain remission. Treatment depends on the disease severity (mild, moderate, or severe), extent, and stage (exacerbation or remission). At first, your doctor will treat the attack by relieving the symptoms and giving the colon a chance to heal. Then, the treatment will aim to maintain this remission as possible and prevent any complications. Acute severe ulcerative colitis may need hospitalization.
If the medical treatment failed to control the disease, surgery would be the choice. Surgery may be urgent in acute attacks or life-threatening complications. Surgery cures ulcerative colitis, but the extraintestinal symptoms persist. Thus, discuss the risks and benefits of surgery with your doctor before a decision.
Medications
We have several medications to use for ulcerative colitis, and the choice depends on the doctor’s evaluation. These medications include:
- Aminosalicylates, such as sulfasalazine, are anti-inflammatory agents with significant effects on ulcerative colitis. They are the first choice in mild and moderate cases. You can take them as suppositories, enemas, and oral forms. The route of administration depends on the disease’s extent.
- Corticosteroids, such as prednisone, might be used if the aminosalicylates failed to control the symptoms (moderate to severe cases). Due to their several side effects, their usage should be for a short period.
- If the previous anti-inflammatory agents didn’t give the desired response, your doctor might use immune system suppressors, such as azathioprine. These medications reduce inflammation by suppressing immune functions, which can lead to severe side effects. They take some time to work. Also, these drugs need frequent evaluation to notice any of their side effects.
- Biologics, such as infliximab, also may be a choice in severe cases and those that don’t respond to the previous medications. But, they also need close monitoring due to their several severe side effects.
- Symptomatic treatment includes:
- Antidiarrheal agents
- Analgesics
- Antispasmodics
- Antibiotics (for infections)
- Iron supplementation (for anemia)
Only take what the doctor prescribed to you because these medications may cause severe adverse effects, and your doctor will weigh the risks and benefits according to your case.
- Surgery
It cures ulcerative colitis, but it requires removing the entire colon and rectum, which may need you to wear a bag to collect your stool through an opening in your abdomen. In some cases, the surgeons can make a pouch from the end of the small intestine and attach it to the anus.
Surgery may be urgent and necessary, such as in:
- Uncontrolled bleeding
- Perforated colon
- Toxic megacolon resistant to the medical treatment
- Severe attacks that don’t respond to medical treatment
- Suspected cancer
Other than life-threatening conditions, surgery is elective, depending on your case. Your doctor will decide the best surgical procedure for you, either total removal of colon and rectum, colon only, or only part of the colon.
Finally
As you can see, ulcerative colitis has no standard treatment for all cases. Commit to the plan of your doctor. Also, revise your doctor for any new complaints or worsening because you may need to change the treatment due to poor effects or side effects. An efficient control plan means better quality of life and a low risk of life-threatening complications.