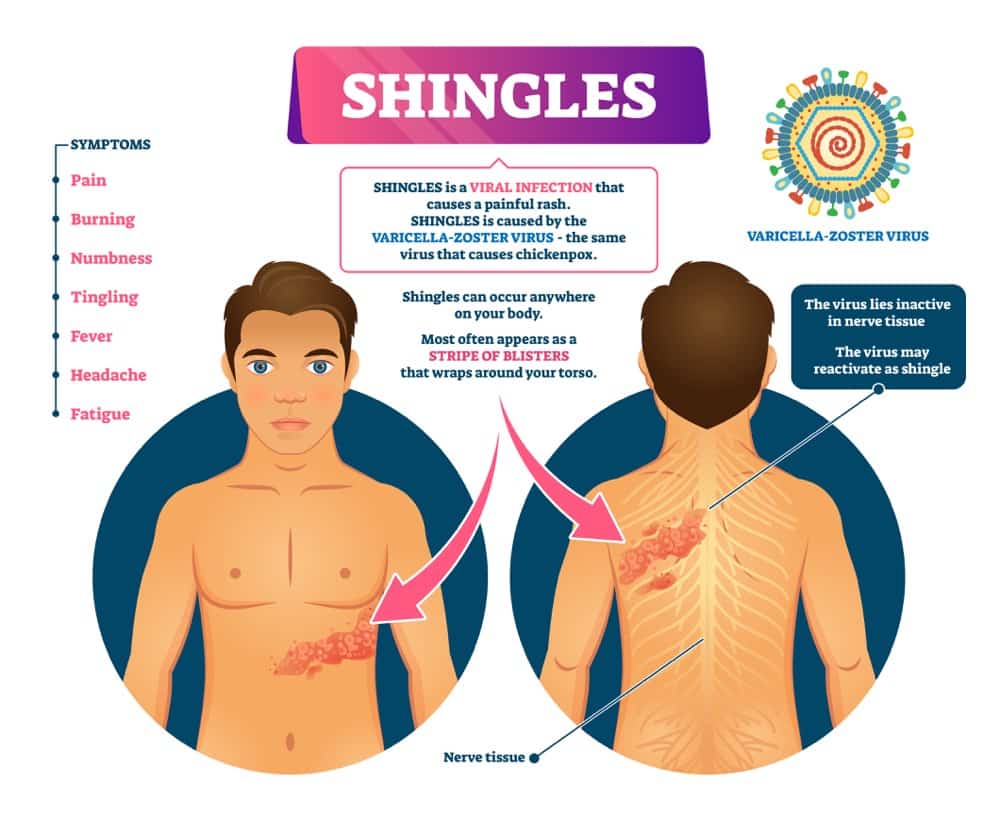
“Shingles” is the most common name to call a viral infection known as herpes zoster. This infection starts in the skin but also includes the nervous system because it travels to sensory nerves and stays latent for months, years, or a lifetime.
It is an acute disease triggered by a reactivation of the varicella-zoster virus. In other words, these patients will have a history of varicella infection that healed already and then reactivated into this skin manifestation.
The reason why herpes zoster comes back after months or years is probably due to a problem in the patient’s immune system. The virus detects a chance of replication when the immune system is affected and starts doing so right away. Stress, infections, and certain drugs may induce herpes zoster in patients with previous varicella infection.
Interestingly, most patients with shingles will have a normal immune response. They are not necessarily immunocompromised, and not all of them have chronic diseases or go through immunity challenges. In such cases, the condition probably happens because of a transient drop in antibody titers against the varicella-zoster virus.
Shingles have different forms and manifestations. It is not always the same dermatomal rash. Sometimes we can develop a neurologic disease or a severe ophthalmic condition.
Since there are different manifestations of the disease, this time, we have devoted one article to describing the most common signs and symptoms of shingles. We will also cover some of the rare manifestations of the disease, and a few complications patients can experience during the acute phase.
The following are the most critical symptoms we should look for in patients with shingles:
1. Skin hypersensitivity
In most cases, the first manifestations of the disease include a prodromal syndrome characterized by sensitivity changes in the skin. Patients typically feel pain in a specific area that corresponds to the reach of a single nerve. These regions are uniform and depend on body anatomy. Therefore, they can be detected by a skilled physician as dermatomes. Hypersensitivity in dermatomes can be reported as pain or itching. It is one of the first manifestations of the disease and lasts around 48 hours.
2. Malaise
The prodromal syndrome also includes a sensation of unrest or not feeling well. This can be reported as general weakness or very mild pain in the body. In any case, patients feel a reduction of energy, and they realize there’s something wrong.
3. Myalgia
Body pains are also common in the prodromal stage of the disease, which is limited to the first week and up to 10 days. Myalgia is the clinical name of muscle pain, which is usually accompanied by malaise and body weakness. It usually resolves by itself but can also improve with anti-inflammatory medications.
4. Headaches
This symptom is also included in the prodromal syndrome of shingles. However, depending on the area and type of herpes zoster, headaches can become an important symptom throughout the disease. For example, when herpes zoster takes the trigeminal nerve, it causes severe headaches, toothaches, and other symptoms we will cover later in this article.
5. Photophobia
This symptom is not the most common in the prodromal syndrome of shingles, but it can sometimes happen in patients, especially those with ophthalmic or cranial nerve involvement. They may increase their sensitivity to light, which is known as photophobia. In some cases, they suffer from migraines, and light becomes a trigger of headaches. After the prodromal syndrome, photophobia becomes prevalent in patients with ophthalmic manifestations of the herpes virus.
6. Fever
This symptom is rare in the prodromal stage of shingles. It usually happens when there’s an infection overlapped with the initial manifestations of the disease. But it sometimes accompanies myalgia, headaches, and malaise in the initial phase of the disease.
7. Vesicular skin rash
Skin rash is by far the most important manifestation of the disease. In some cases, the skin rash in herpes zoster is similar to herpes simplex. In others, it is entirely different and does not feature the same symptoms. A similar manifestation arises in patients with a vesicular skin rash. They develop vesicles limited to the reach area of the affected nerve. The skin rash develops in dermatomes, which can be evaluated and identified by a skilled physician. They are vesicles filled with a clear liquid which then cloud and burst. This shows up after the prodromal period and is associated with pain and hypersensitivity.
8. Skin ulcers
The vesicles in the skin rash do not stay the same throughout the disease. The liquid initially clouds and does not look clear anymore. After that, the vesicles tend to burst, leaving a sort of ulcer on the skin. This open wound would then crust and slowly involute.
9. Pain without vesicles
In some cases, patients would describe the typical pain of herpes zoster without skin rash. They may not have any vesicles at all, or maybe they have a reddened area in the skin and nothing more. This is also likely in some patients and can be a manifestation of the reactivated viral infection.
10. Patchy erythema
There’s also the possibility of developing patchy erythema instead of vesicles with fluid. As the name implies, patchy erythema looks like a reddened skin region in patches. In some cases, these patches are also indurated. In other words, the skin becomes slightly hardened. All of these manifestations, including patchy erythema, are limited to the affected dermatome corresponding to the nerve initially taken by the disease.
11. Enlarged lymph nodes
Swollen lymph nodes are also likely in these patients. This is known in medical terms as lymphadenopathy, and it is located around the affected skin area. Other body parts are not taken. For instance, a patient with a herpes zoster skin rash around the ribs on the right side may develop enlarged lymph nodes in the right armpit. The left armpit and the groin will not develop lymph nodes. Enlarged lymph nodes may show up at any stage of the disease, except for the prodromal phase.
12. Scarring
As noted above, the skin rash in herpes zoster tends to go through different phases. It starts by showing up vesicles that cloud and burst. They crust and slowly involute. In most cases, they won’t leave a trace. In others, it could leave a scar depending on the patient’s habit of scratching and the existence of a secondary infection.
13. Secondary infections
This is a type of complication in herpes zoster because it is not the usual course of the disease. It is a secondary skin rash infection, and it usually happens once the vesicular lesions burst. People who develop secondary infections typically have the habit of scratching, bursting the vesicles, removing the crust of lesions, or using tight clothes. Manipulation is the most common cause of secondary infections. It also happens, and sometimes spontaneously, in patients with HIV and other immune deficiencies.
14. Postherpetic neuralgia
Patients can be left off with pain in the dermatome even after the skin rash is gone. This pain is known as postherpetic neuralgia, and it is a nerve-related pain with no skin changes. Postherpetic neuralgia can linger in these patients for weeks or months. In some cases, patients can still have the symptom after years of the initial manifestation of herpes zoster. The pain tends to be severe and does not respond to the usual pain medications because it is a nerve-related pain and not associated with inflammation. Patients with severe pain in the eruptive phase of the disease and a higher density of herpetic eruptions are more likely to endure postherpetic neuralgia after the skin rash is resolved.
15. Pain and symptomatic recurrences
After being apparently cured, herpes zoster can strike again and cause a new episode. This is known as recurrent herpes zoster. It doesn’t happen to every patient, and it is luckily a rare occurrence, with 12 cases per 1000 person-years. Recurrent herpes zoster will be more likely in patients aged 51 or older and when the initial manifestations of herpes zoster, including pain, were maintained for 30 days or more.
16. Ophthalmic manifestations
It is known as herpes zoster ophthalmicus, resulting from the invasion of the Gasser ganglion. This type of herpes zoster happens in 10-15% of patients and includes many ophthalmic lesions, including conjunctivitis, keratitis, scleritis, retinitis, and optic neuritis. Most of the manifestations are inflammatory processes, but other symptoms include lid retraction, ptosis, exophthalmos, and glaucoma. Some patients will also have muscle palsies around the eyes. Patients usually have skin lesions in the forehead and other areas of the affected dermatome. This manifestation of herpes zoster can be very dangerous and leave long-lasting visual impairments when not adequately treated.
17. Intraoral manifestations
In the oral cavity, herpes zoster produces mucocutaneous lesions and a vascular eruption in the area. It is usually associated with vesicles inside the ear and sometimes hearing loss, depending on what nerve it affects. When the maxillary division of the trigeminal nerve is taken, it can cause periodontitis and other tooth-related problems.
18. Herpes zoster oticus
This type of herpes zoster affects the ear canal and the inner ear when the geniculate ganglion is infected with the virus. It is not the most common manifestation of the disease. The signs and symptoms include ear pain or otalgia and vesicle formation in the tympanic membrane or the ear canal. These patients likely have auditory problems ranging from mild impairment to complete deafness. They sometimes have balance problems if the disease takes the vestibular chambers of the inner ear.
19. Encephalomyelitis
When herpes zoster affects the brain and its membranes, it causes inflammation of the brain structures, known as encephalomyelitis. These patients have neurologic problems and may sometimes develop a type of meningitis with symptoms such as headache, fever, neck stiffness, and sensory changes. Symptoms of herpes zoster encephalomyelitis can be severe, and it is a cause of fatal hemorrhages and death in some cases. It is sometimes confused with poliomyelitis.
20. Disseminated disease
Most cases of herpes zoster follow the pattern described above, and they are limited to the reach of a given nerve. But some patients develop a disease that is not limited to dermatomes, and it is known as disseminated herpes zoster. It happens in 2% of cases of herpes zoster, but it is more common in immunocompromised patients. It is very difficult to differentiate from chickenpox or varicella. These patients develop more than ten vesicles outside the dermatome taken by the virus, and it develops one or two weeks after the classic manifestations of herpes zoster. In patients with disseminated disease, it is essential to rule out a cause of immunodeficiency, including HIV but also cancer and cancer treatment.
21. Cystitis and other urinary bladder symptoms
When herpes involves the urinary bladder, the manifestations are also vesicles, but they can be in the urinary tract and mucosa of the urinary system. Signs and symptoms in these cases include severe dysuria, described as a burning pain when urinating, and a significant increase in the urinary frequency. In some cases, patients may develop severe cystitis with hematuria or blood in the urine. This happens when the vesicles rupture. In some cases, patients may also develop bladder paralysis and urinary retention.
22. Motor complications
In most cases, the virus responsible for shingles only invades sensory nerves. But the affected ganglion also has a motor component, and the viral particles sometimes cross this area and cause motor problems. Motor complications manifest as muscle weakness or paralysis depending on the severity of the problem.
Luckily, the last manifestations described in this article are not the most common. This disease is usually self-limited, and the signs and symptoms resolve by themselves and without medical intervention. They are generally mild in children and more severe in adult patients.
Management of the disease usually involves providing relief to the symptoms with anti-inflammatory medications, wet dressings, lotions, and other topical treatments. Patients may require anticonvulsant and antidepressant treatment when pain symptoms are more severe. Antiviral therapies may also help reduce the rate of vesicle formation.