Psoriasis and arthritis are thought to be separate health problems, and they apparently don’t have much in common. Psoriasis is a skin problem featuring reddened and scaly plaques in the trunk, scalp, knees, and elbows. Arthritis is a joint pain problem caused by inflammation in the affected articulations and is often associated with degenerative and progressive changes.
But in some cases, arthritis can be one of the manifestations in people with psoriasis. It is not a problem all people with psoriasis encounter, but when it happens, it is known as psoriatic arthritis.
This article reviews the most important data about psoriatic arthritis, including the basic concepts, signs and symptoms, causes, prognosis, and more.
What is psoriatic arthritis?
Psoriatic arthritis is a type of inflammatory disease in the articulations that occurs in patients with psoriasis. It is a chronic disease involving the articulations and the part of the tendon attached to the bone, known as entheses. It is classified as a seronegative oligoarthritis because the patients test negative for the rheumatoid factor in the blood and other arthritis markers, and it affects more than one joint but less than four.
In most cases, psoriasis starts years before the onset of arthritic symptoms. But in some cases, arthritis precedes psoriasis, and still, other patients have both problems simultaneously.
In any case, the diagnosis of psoriatic arthritis follows a list of classification criteria known as CASPAR, and even though there are no tests to diagnose the disease, patients usually need to evaluate their erythrocyte sedimentation rate, C-reactive protein, uric acid, and synovial fluid cell count to guide the management of the disease. Another valuable tool for the diagnosis is radiographic studies to detect the abnormalities characteristic of the disease.
These variations and the need for specialized exams to diagnose the disease are the reasons why psoriatic arthritis was first associated with psoriasis and distinguished from rheumatoid arthritis in the 1960s. Even now, defining psoriatic arthritis precisely can be difficult because there are no specific biologic tests.
Risk factors and causes of psoriatic arthritis
We can consider some risk factors that increase the likelihood of psoriatic arthritis in patients with psoriasis. They include:
- Scalp or nail psoriasis: According to the available data, psoriatic arthritis is more common in patients with psoriatic lesions in the scalp and nails.
- Family history of psoriatic arthritis: If your parents or another family member has psoriasis and develops psoriatic arthritis, your disease may also progress into this inflammatory condition.
- More severe disease: The onset of psoriatic arthritis is more common in patients with more severe disease manifestations.
The exact cause and mechanisms of psoriatic arthritis are not entirely understood. However, we know that genetic factors play a significant role, especially when paired with some environmental factors. Patients may also have an immune component that contributes to the development of the disease.
The proposed causes include:
1. Genetics
There is a significant genetic factor that increases the susceptibility of psoriatic arthritis in patients with psoriasis. This is highlighted by the fact that 40% of patients with psoriatic arthritis have relatives with the same disease. Studies have found some genes that can be involved in the development of the disease. Most of them are members of the HLA family, including HLA-B7, HLA-DR4, and HLA-B27. Additionally, some gene polymorphisms can be associated with the disease, especially those in the TNF promoter region.
2. Immunologic factors
The inflammatory joint disease in psoriatic arthritis is led by immunologic factors. Different inflammatory cytokines are elevated in these patients, including IL-6, IL-1, and IL-8 in the synovial fluid and TNF-alpha in the blood. In this regard, the disease is similar to rheumatoid arthritis. The immunologic cause is probably related to activation of inflammation mediated by T helper 17 cells.
3. Environmental triggers
There are environmental factors that trigger psoriatic arthritis and psoriasis. In most cases, they include a viral or bacterial infection. In other cases, they are triggered by trauma. Moreover, bacterial infections can exacerbate the symptoms in patients already diagnosed with psoriatic arthritis.
How common is psoriatic arthritis?
One in every five patients with psoriasis develops psoriatic arthritis. However, as noted above, some patients with psoriasis are more likely to experience this problem. One of the most important risk factors is the severity of the skin disease.
According to statistics, 54.9% of patients with severe psoriasis progress to psoriatic arthritis. That is more than half. In moderate psoriasis, 35% of the patients develop these joint manifestations, and the incidence is 9.9% in patients with mild psoriatic arthritis.
In the United States, the incidence of psoriatic arthritis is 30% in people with psoriasis, which is close to 1 million people. However, other studies report different statistics, and the exact frequency is 5-30% depending on the study and the population.
Worldwide, the incidence of psoriatic arthritis is 133 patients per 100,000 population. That is to say that one in four patients with a diagnosis of psoriasis develops psoriatic arthritis. The incidence is exceptionally high in sub-Saharan Africa, especially among people with HIV.
The age of onset is usually between 35 and 55 years. There is also a juvenile form of psoriatic arthritis in patients aged 9-11 years. It is more prevalent in whites, but African Americans usually have worse symptoms if they develop the disease.
Is it a dangerous disease?
What happens with people suffering from psoriatic arthritis? The disease is not life-threatening in most cases. Most patients have mild arthritis without deformation, but 40% develop a more severe illness with the destruction of articulations. Still, not all patients require musculoskeletal surgery and other invasive procedures to control psoriatic arthritis.
The mortality rate in psoriatic arthritis is almost the same compared to healthy patients. Thus, we can say that it is not a particularly dangerous disease. However, these patients are more likely to have hypertension, diabetes, obesity, altered blood lipids, and cardiovascular disease. There is also a higher prevalence of gastrointestinal disorders, liver disease, neurologic conditions, and infections in patients with psoriatic arthritis.
The disease appears not to pose a risk for pregnant women, and studies show that disease activity decreases during pregnancy. After giving birth, the severity of the condition returns to the usual pattern in a matter of months.
Signs and symptoms
The onset of psoriatic arthritis is usually around ten years after the onset of psoriasis. However, the age of onset influences how destructive psoriatic arthritis can be. When the disease starts in patients after 60 years, the beginning is more severe, and the condition is usually more destructive, associated with more severe manifestations.
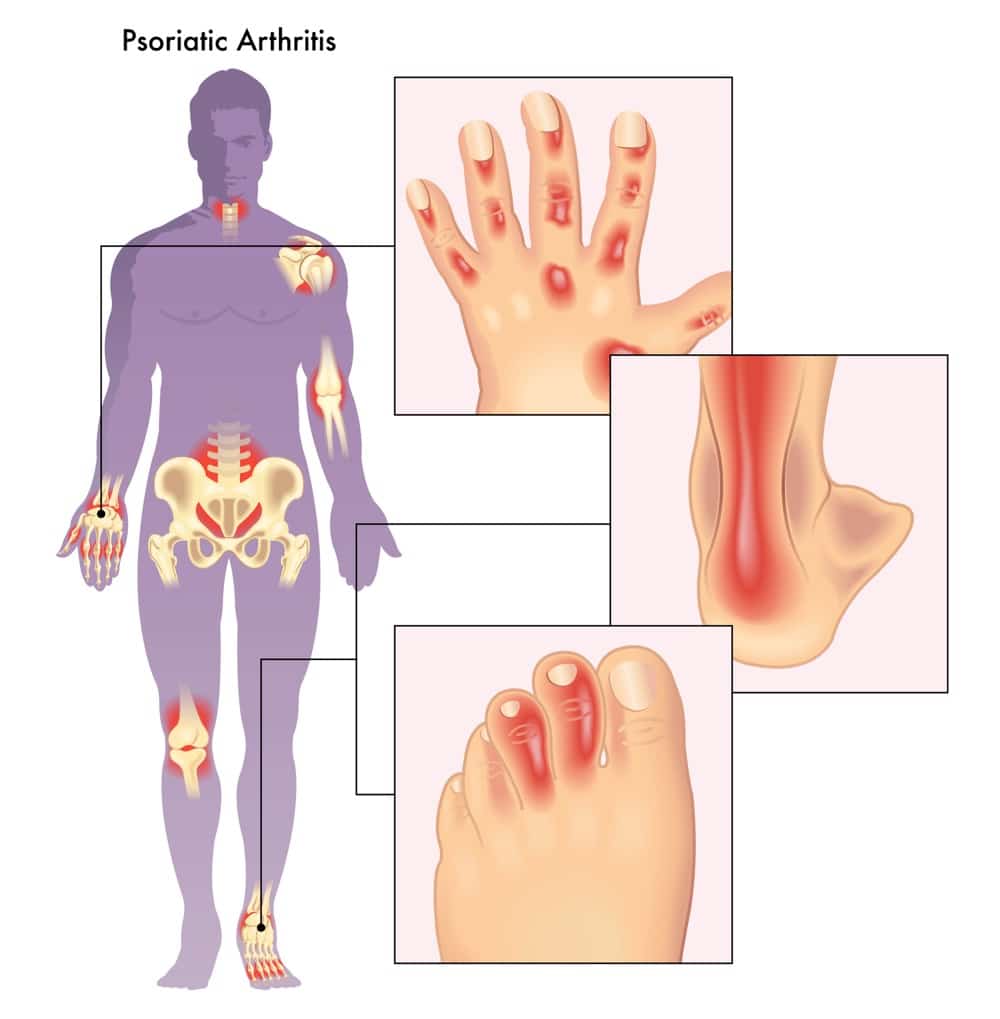
Most patients with psoriasis have problems in the peripheral joints, especially in the hands. But in 5% of patients, the axial spine and other central joints are involved. So, the following signs and symptoms are usually related to the hands and peripheral joints, but others can also be involved.
The most important signs and symptoms in arthritic psoriasis include:
1. Psoriasis signs and symptoms
In 60-80% of cases, psoriasis precedes psoriatic arthritis. Patients may start showing joint involvement a few years after the onset of arthritis. They already have the signs and symptoms of psoriasis. A minority of patients develop arthritis before psoriasis or have both conditions simultaneously. The skin lesions are usually located in the scalp or nails.
2. Different patterns of joint involvement
Patients may develop different patterns of joint involvement. The most common are asymmetrical oligoarticular arthritis, with more than one and fewer than four articulations taken in a symmetric pattern; symmetrical polyarthritis, with more than four articulations taken in a symmetric pattern; distal interphalangeal arthropathy, when only the hands are affected by the disease; arthritis mutilans, when joint destruction is prevalent, and the function is compromised by the deformity.
3. Joint pain
This is probably the most important symptom in arthritis in general and psoriatic arthritis in particular. The onset of the pain symptoms is insidious and progressive. But one-third of patients develop a sudden onset of moderate or severe joint pain from the initial stage of the disease. Most patients develop joint pain in the articulations of the limbs, but some experience problems in the spine and other articulations of the trunk.
4. Stiffness
Along with pain, most patients experience stiffness in the affected articulations. The problem is worsened when psoriatic arthritis causes deformity in the articulations.
5. Tenderness
In other words, when touching the articulation, patients experience more pain than the baseline. This symptom is prevalent in psoriatic arthritis, but it is not as severe as rheumatoid arthritis.
6. Enthesitis
In other words, the inflammation of the structure that joins the tendons with the bone. Since tendons are affected by the disease. The pain is not necessarily limited to joints. It can also affect large tendons such as the plantar fascia and the Achilles tendon.
7. Dactylitis and sausage digits
In 35% of patients with psoriatic arthritis, they develop severe inflammation and swelling in the hands. The distal interphalangeal joints are taken, and the nails are deformed. This gives the appearance of sausage digits.
8. Nail changes
Up to 80% of patients develop various nail changes. These changes include oil spots, beau lines, splinter hemorrhages, cracking of the edges, nail pitting, and other alterations. In most cases, extensive nail involvement is associated with more severe deforming arthritis in the hands.
9. Subcutaneous nodules
It is rare, but some patients also develop subcutaneous nodules and psoriatic arthritis. These cases should be evaluated to rule out the occurrence of rheumatoid arthritis and psoriatic arthritis.
Treatment options
Treating psoriatic arthritis has the primary goal of controlling inflammation in the articulation and treating the skin manifestation of psoriasis. In some cases, patients with deformations may also need correction of their articulations and treatment with antirheumatic drugs and biologic agents. Surgical interventions are limited to patients with severe contractures and pain, with movement limitations caused by joint deformation.
In short, the treatment of psoriatic arthritis includes:
1. Medications
It is important for symptomatic relief and includes non-steroidal anti-inflammatory drugs. However, some patients may also require injections with glucocorticoids. Others improve their symptoms after using oral glucocorticoids. As noted above, some patients may require a more aggressive approach, primarily when the disease is associated with joint deformation. These patients may require methotrexate, cyclosporine, and other antirheumatic drugs. In some cases, doctors may also recommend biological therapy.
2. Physical therapy
It should be included at the beginning of the disease to prevent a progressive worsening of the condition. It should be used as long as patients tolerate it. In some cases, physical therapy is replaced by guided exercise. It should be low-impact exercises such as swimming, yoga, and tai chi. The rehabilitation process depends on the stage of the disease and the severity of the manifestations. Physical therapy may include stretching and strengthening exercises, heat and cold therapy, and assistive devices to aid patients in their gait.
3. Lifestyle changes
Some lifestyle changes may also reduce the burden of the disease. One of the most important recommendations is smoking cessation. Weight loss is also recommended in overweight and obese patients because this extra weight places additional stress on the affected joints. Thus, living a healthy lifestyle should be a general rule for these patients to improve their own quality of life. Rest is also essential, especially in acute episodes when the pain increases. It may also be useful to explore vocational readjustments in patients who work in a very active environment.
4. Surgery
It only treats severe diseases. For instance, arthroscopic synovectomy can be a treatment for monoarticular synovitis. Joint replacement therapy and other reconstructive surgeries are helpful in the case of knee and hip involvement. In arthritis mutilans, patients may also receive arthroplasty, arthrodesis, or bone grafts.
Conclusion
Psoriatic arthritis is an inflammatory disease of the articulations in patients with psoriasis. It can be mild or severe, with deformity and destruction of the articulation in the worst-case scenario.
Symptoms are similar to rheumatoid arthritis, including pain, stiffness, and tenderness in the affected articulations. The treatment usually involves a combination of physical therapy and pain medications. In some cases, patients may also require antirheumatic drugs and biologic therapy. Surgery is reserved for patients with severe involvement of the articulations, deformity, and functional limitations.