Pancreatic cancer is one of the worst diseases a human can be diagnosed with. The reason is usually the fact that the vast majority of patients are diagnosed late, too late for surgery to be curative. Surgery is the only curative treatment for pancreatic cancer, and patients who are not eligible for surgery are unlikely to live for long. However, if cancer is caught early, usually before the clinical appearance becomes full-blown, surgery becomes a viable option and patients can be disease-free for years with much higher survival rates. In this article, we will talk about pancreatic cancer, its causes, its symptoms, how it is diagnosed, and how it can be treated. Raising awareness of pancreatic cancer can help many sufferers pick up symptoms early on and save their lives.
Our pancreas, the hidden organ:
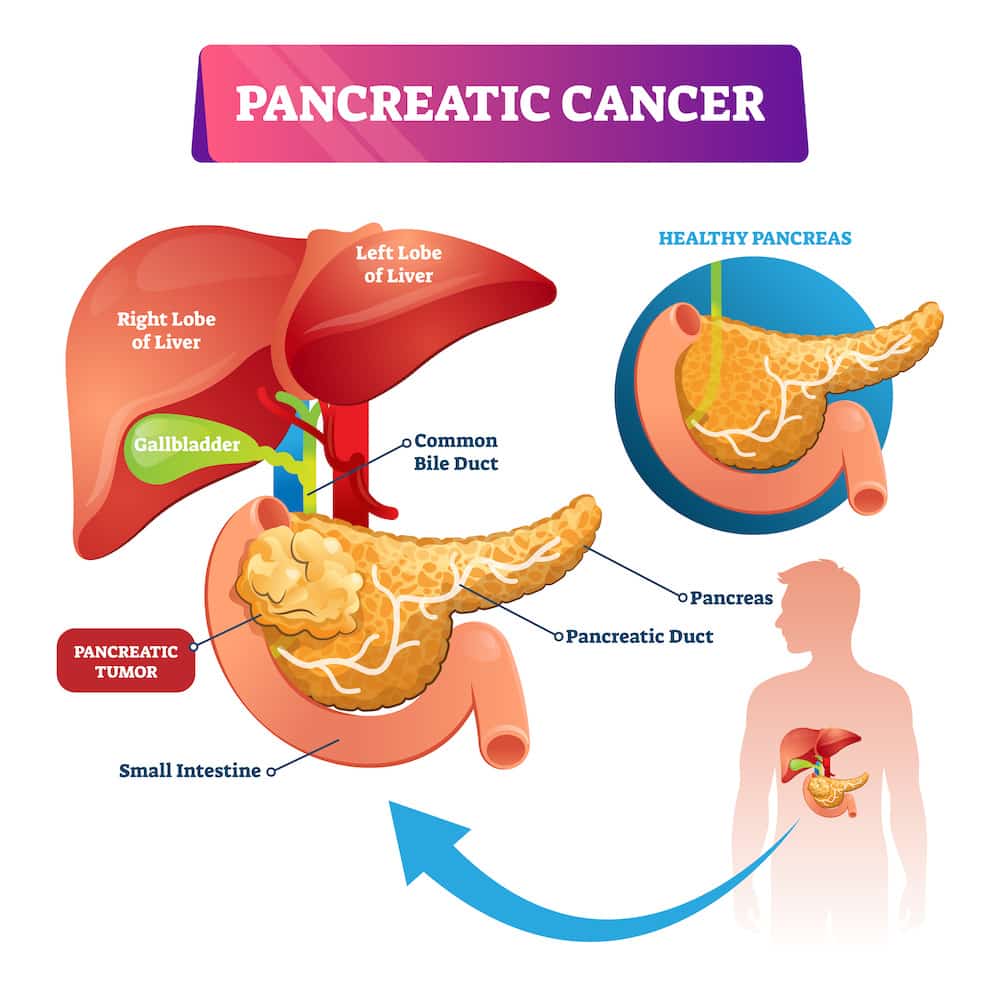
The pancreas is a unique organ found at the back of our abdominal cavity. It is located just behind the stomach and is surrounded by various blood vessels, so its cancer can be incurable if it extends to invade them. The pancreas consists of a head, neck, and tail. The head is the part closest to the gastrointestinal tract and contains glands that secrete digestive secretions, while the tail contains other glands that secrete insulin and glucagon. Both of those hormones are crucial to controlling blood glucose levels. The pancreas had long been unapproachable by surgeons owing to its fragility and complications from its surgery. One famous surgeon was even quoted to say, “God placed the pancreas at the back of the abdomen so surgeons wouldn’t mess with it”. However, this view has long changed and it is now operated upon in many conditions with minimal complications.
How common is pancreatic cancer, and what causes it?
Pancreatic cancer is the tenth most common cancer in humans and is the 4th leading cause of death from cancer, proving that it is one of the most lethal cancers. Most pancreatic cancers occur in the head or neck and a minority occurs in the tail, and these are good news as will be explained later.
Unlike other diseases, it isn’t always easy to put causes for cancers owing to the complexity of their development. Instead, we put a number of risk factors that interplay whether all or some of them to develop that specific type of cancer. In the case of pancreatic cancer, these risk factors include:
- Smoking: Smoking is the most identifiable risk factor for pancreatic cancer, and smokers are at increased risk of developing it the longer they smoke.
- Diabetes: Although the cause is not yet well known, diabetics are at an increased risk of developing pancreatic cancer.
- Obesity: Although not as pronounced as smoking, obesity is a known risk factor for pancreatic cancer.
- Family history of pancreatic cancer: About one in ten cases of pancreatic cancer is related to family history.
- Alcohol consumption: Alcohol consumption is one of the risk factors, too, and it is not well known whether it is because of the alcohol itself or chronic pancreatitis, which is a chronic inflammation of the pancreas from several causes including alcohol.
Symptoms of pancreatic cancer:
Pancreatic cancer has a high tendency to be clinically silent, and the condition can become incurable before showing any significant symptoms. Furthermore, some of its initial symptoms can be mistaken for other conditions or simply ignored by patients. That is why it is important to know the symptoms that should prompt you to visit your doctor and seek a further assessment.
The main symptoms of pancreatic cancer are:
- Abdominal pain: The pancreas is located in the abdominal cavity, and its involvement in any condition whether inflammation, infection or cancer causes a special type of pain which is located at the upper center of the abdomen and radiates to the back. This pain usually worsens when you lie on your back. It may also be worse at nighttime.
- Nausea and vomiting: Although not a specific feature of pancreatic cancer, a general sense of loss of appetite, nausea, and vomiting can occur with pancreatic cancer.
- Loss of weight: One of the most alarming symptoms of cancer in general and pancreatic cancer, in particular, is the acute loss of weight. Loss of weight may be attributed to decreased appetite, but more importantly, it shows that a mass is consuming food material at an accelerated rate, signifying the risk of ongoing cancer.
- Generalized sense of weakness: A generalized sense of weakness may also be a symptom of cancer. Losing blood from cancer into the gastrointestinal tract can cause severe anemia, which causes weakness and intolerability to effort.
- Jaundice: Among all the symptoms of pancreatic cancer, jaundice is the most specific yet the latest. It occurs when the pancreatic cancer of the head obstructs the flow of bile into the small intestines. The bile then regurgitates back into the blood and causes the deep yellowish tinge of the skin, eyes, and lips.
- Diabetes: Although diabetes is not a symptom, people who have been diagnosed with diabetes recently and who have one or more of the above symptoms should check themselves for pancreatic causes of diabetes including cancer.
- Itching: When pancreatic cancer obstructs the bile duct, regurgitation of bile salts into the blood causes severe skin itching, a condition known as pruritis. Although pruritis occurs in all cases of jaundice due to obstruction, it is most pronounced in pancreatic cancer.
How will my doctor diagnose cancer?
Specific symptoms suggesting pancreatic cancer should alert the physician towards its possibility and they will order a battery of laboratory investigations and -more importantly- imaging studies.
Laboratory investigations aim at identifying the cause of jaundice as well as assessing anemia if present, while imaging studies detect the mass and its extent.
Laboratory investigations include:
- Complete blood count: A complete blood count is routine in most medical conditions, but in pancreatic cancer, it helps detect anemia when the level of hemoglobin falls.
- Bilirubin: Bilirubin is the cause of jaundice and includes two subtypes, direct and indirect. When direct hemoglobin increases at the expense of the indirect, it shows that an obstruction is present, while if the indirect is higher, it shows that the cause is either in the blood or the liver.
- Tumor markers: Tumor markers are chemical substances mostly secreted by cancer. They are usually present normally in the body but at very low levels, and an increase in their level is indicative of cancer. They are also used to detect whether cancer has been effectively eliminated after surgery. In the case of pancreatic cancer, its tumor marker is called CA19-9.
Imaging studies
Several imaging studies can help visualize pancreatic cancer including:
- CT scanning: Abdominal CT scanning is the most specific investigation for pancreatic cancer. It shows its size, location, and whether or not it invades the surrounding structures and blood vessels.
- Ultrasonography: Ultrasonography is not specific for pancreatic cancer, but it is usually the first imaging study done if the diagnosis of jaundice is not sure to exclude causes in the biliary tract and liver.
- ERCP: ERCP is one of the investigations done to detect any anomaly of the biliary tract. It is an invasive procedure that involves doing an endoscopy then injecting a dye into the biliary tract. It can differentiate between the different causes of jaundice.
- MRCP: It is similar to ERCP, but no dye nor an endoscope are used. It is similar to MRI of the brain and spinal cord and uses magnetic waves instead of contrast material and radiation.
Is pancreatic cancer treatable?
Although pancreatic cancer is a grim diagnosis, it is not incurable. Cancers in general are not completely curable because the main defect behind their development -genetic defects- is always present. The measure of curability, therefore, is not the complete disappearance of all cancerous genetic material but the absence of a visible tumor or detectable cancerous cells. Another important measure is the survival rate, which is the percentage of patients still alive after a certain amount of time following diagnosis. Regarding pancreatic cancer, the survival rate of patients is 20% for 5 years.
The only curative option for pancreatic cancer is surgery, which is usually only possible in cancers of the head, owing to the fact that they cause most symptoms mentioned above at an early stage, allowing for surgery to take place. Cancers of the tail, on the other hand, rarely present early on, delaying the diagnosis past the viability of surgery. The operation commonly done for pancreatic cancer is called Whipple’s operation, which involves the removal of the pancreatic head, the duodenum -the first part of the small intestines-, and the bile duct. Whipple is only done for cancers of the head, while body and tail cancers are usually treated by the complete removal of the pancreas (pancreatectomy).
Other treatment options:
Although surgery is the only curative option for pancreatic cancer, chemotherapy has a significant role in therapy. Chemotherapy can be used either before or after surgery or in cases of irresectability. Chemotherapy is given before surgery can shrink the tumor or displace it away from vital structures, making it respectable. Giving chemotherapy after surgery ensures that any metastases -a few cancerous cells that move by blood to other parts in the body- are eliminated. Chemotherapy can be palliative to reduce tumor size and complications.
Surgery is not always curative, too, and it can be palliative to reduce tumor size or to destroy a part of the nervous system called a celiac ganglion, which carries sensation from the pancreas. It is the last resort in pain relief. Other options for pain relief and palliation include using strong analgesics.
Patients who suffer from jaundice and are not eligible for curative surgery can undergo a procedure called stent placement. An endoscopy is done similar to ERCP, but a metallic stent is placed to permanently widen the bile duct and allow the bile to flow.
How likely am I going to survive if my pancreatic cancer is inoperable?
To answer the question of survival after cancer, a few concepts need to be established:
- As mentioned above, the measure of survival is the 5-year-survival rate. However, surviving for more than 5 years following diagnosis does not mean a cure. Patients can have a recurrence any time following initial diagnosis and treatment. That is why follow-up both by clinic visits and imaging studies is essential for patients recovering from pancreatic cancer.
- Survival is not only related to the treatment received. Although early surgery is crucial to long term survival, individual factors like age, general health and the
- the aggressiveness of primary cancer.
It is quite difficult to place a solid number for months of survival following treatment. Only about a fifth of patients are eligible for surgery at the time of diagnosis, and in those patients, only 20% can live for more than 5 years. In those patients who had already developed advanced disease or metastases (systemic spread of cancer), the median survival is 6 months.
Should I worry that my abdominal pain may be pancreatic cancer?
One of the side effects of reading about a certain condition is that you might think you have it if you developed a symptom of it. The rarity of a condition is important in these cases, and we have to understand that no matter how common cancer is, it remains an improbable diagnosis from a single symptom. Doctors go through many diagnoses before reaching a final one, and many investigations may need to be done in doubtful cases. The purpose of this article is not to alert you unnecessarily but to enlighten you regarding a certain condition. For the sake of knowledge, all of these diseases can present as abdominal pain similar to that of pancreatic cancer:
- Acute pancreatitis: An inflammation of the pancreas.
- Chronic pancreatitis: A condition resulting from chronic alcoholism.
- Abdominal aortic aneurysm: A distension of the main artery passing through the abdomen.
- Gall bladder conditions
- Liver inflammation and cancer
- Intestinal conditions as ischemia: Intestinal ischemia is the acute or chronic diminution of blood supply to a segment of the intestines.
That is why you should visit your physician whenever an alarming symptom develops and not worry excessively about any condition until it is diagnosed.