We often think about cancer as a solid tumor growing on healthy tissue, usually an organ such as the liver, the prostate, or the mammary glands. But there are also non-solid cancers, and blood cancer is one of them. Multiple myeloma is a type of cancer affecting blood cells. It was initially described back in 1848, and it is actually included in a wide range of blood cell diseases that include plasma cell leukemia.
What is it exactly? Why does it happen? How does it feel? And what treatment options are there available for these patients?
Overview
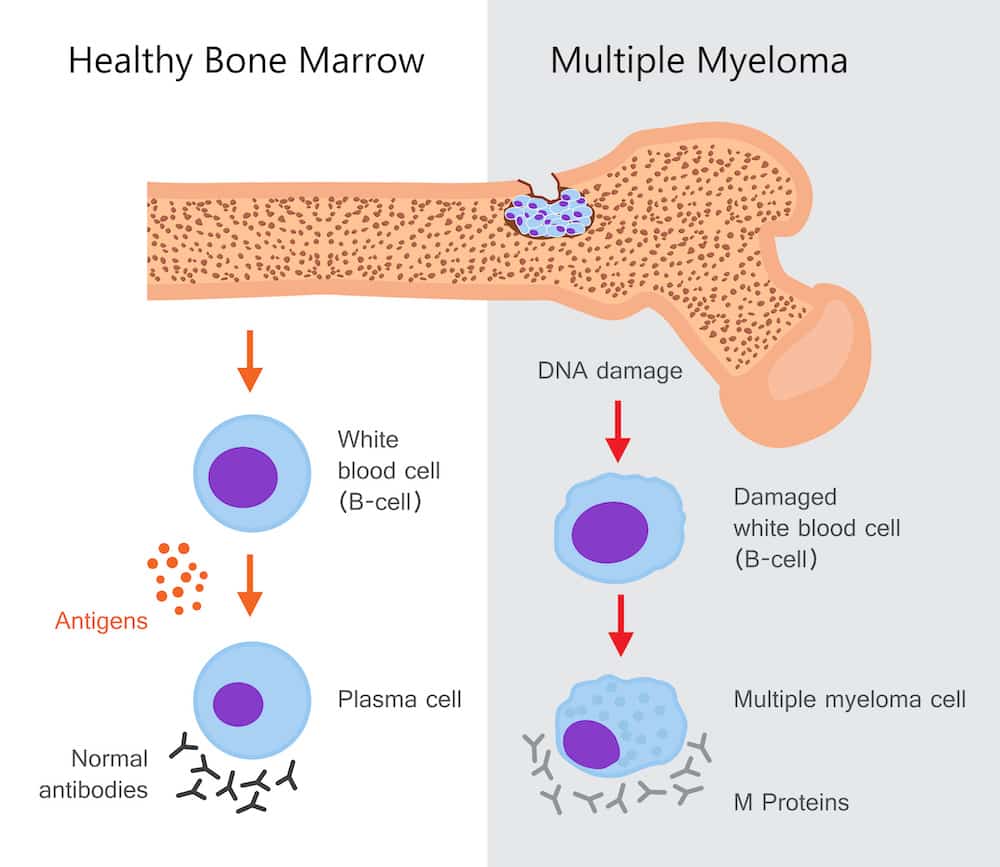
As noted above, multiple myeloma is a malignancy or cancer that affects a type of blood cell known as a plasma cell. In this disease, there is an over-proliferation of monoclonal plasma cells in the bone marrow, which affects the growth and differentiation of other cell lines.
The disease can be asymptomatic sometimes, but other patients report severe symptoms and sometimes complications that require emergency medical attention. The diagnosis is usually made with a routine blood screening, but some patients have a pathologic fracture as the initial finding to diagnose the disease.
There is currently no cure for multiple myeloma. Still, different therapies can be used to control the severity of the disease and its symptoms, preventing the occurrence of complications in the process.
Causes
In multiple myeloma, patients usually start with a condition known as monoclonal gammopathy of undetermined significance. This is a plasma cell condition that precedes cancer, a premalignant condition in which affected plasma cells go through one mutation after the other, increasing their capacity to proliferate rapidly and without any control. In this premalignant condition, plasma cells are still taking 10% of the bone marrow or less.
This is followed by smoldering multiple myeloma, in which the number of plasma cells in the bone marrow goes beyond 10%. In the end, plasma cells in multiple myeloma lose their self-restraints and become aberrant. They have extra copies of chromosomes and many overlapping mutations with impressive genetic heterogeneity. Such variations in proteins and genetic makeup contribute to drug resistance in these patients.
There is no exact trigger for all of these changes, but a variety of factors play a significant role:
- Genetic risk factors: The disease apparently has an important genetic predisposition because it is more common in identical twins and those who have first-degree relatives with multiple myeloma. This is apparently due to abnormalities in specific oncogenes such as c-myc and PT53.
- Environmental risk factors: People who are frequently exposed to herbicides, insecticides, benzene, organic solvents, and other petrochemical industry products are at a higher risk of developing multiple myeloma.
- Patients with MGUS: When patients are diagnosed with monoclonal gammopathy of undetermined significance (MGUS), they are at a higher risk of multiple myeloma than the rest of the population. These patients have a mounting risk of progression to multiple myeloma of 1% every year.
- Radiations: Multiple myeloma has been found at a higher incidence in survivors of the atomic bomb. Similarly, there was a correlation between a higher risk of multiple myeloma in patients exposed to uranium radiation.
- Inflammatory diseases: Patients with inflammatory diseases have a slightly increased risk of multiple myeloma. This correlation is still elusive, and some studies show no association.
- Infections with herpesvirus 8: When human herpesvirus 8 infections affect the dendritic cells in the bone marrow, patients will have a higher risk of monoclonal gammopathy of undetermined significance, which then turns into multiple myeloma.
Signs and symptoms
Multiple myeloma can be symptomatic or asymptomatic depending on the stage of the disease and each particular patient. 30% of cases are detected with a routine blood screening, and these patients do not display any signs and symptoms. The rest of the patients are usually diagnosed after they start displaying bone-related events, usually a pathologic fracture.
Here’s a list of signs and symptoms:
- Bone pain: It is the most common symptom in multiple myeloma, and up to 70% of patients display some degree of bone pain when they are diagnosed. The symptom may not be severe, and it is sometimes neglected by patients. The most usual painful area is the lumbar spine, which is why these patients typically report chronic back pain.
- Pathologic fractures: Up to 93% of patients with multiple myeloma will develop a type of pathologic fracture or a bone lesion in one site or more. This is a widespread finding in multiple myeloma patients and often a cause of evaluations and diagnostic tests in otherwise apparently healthy patients.
- Compression in the spinal cord: In some patients, multiple myeloma has a compressive effect on the spinal cord. This happens in different levels of the spine, and presenting symptoms include numbness, muscle weakness, and back pain. This condition often takes the extremities, and some develop paralysis if the patient is not treated correctly.
- Bruising and easy bleeding: Similar to other blood malignancies, multiple myeloma is associated with an increased risk of bleeding and clotting abnormalities. Not all patients develop this problem, but it is not rare, either. As noted above, multiple myeloma triggers a displacement of hematologic lines and sometimes triggers thrombocytopenia. In other cases, the monoclonal proteins absorb clotting factors and cause a tendency to bleeding.
- Hypercalcemia symptoms: Around 30% of patients with multiple myeloma may also develop an alteration in blood calcium levels. Hypercalcemia is an increase in blood calcium, and patients usually develop symptoms such as constipation, somnolence, confusion, and nausea. Unlike other malignancies, patients with hypercalcemia in multiple myeloma do not affect their prognosis.
- An increase incidence of infections: The displacement of cell lines in the blood causes a deficiency in the number and function of white blood cells. This often leads to infections, especially from microorganisms such as herpes zoster and Haemophilus influenza.
- Blood hyperviscosity: In these patients, blood viscosity is usually higher, sometimes 4 times the blood viscosity of normal patients. This triggers a series of signs and symptoms that include general malaise, somnolence, easy bruising, sluggish thinking, and sometimes fever and sensory loss. In advanced conditions, patients may also develop epistaxis and a higher risk of heart attack, stroke, and other cardiovascular events.
- Neurologic problems: The more rapid multiple myeloma is diagnosed and treated, the less likely it will be to develop neurologic complications such as peripheral neuropathies and carpal tunnel syndrome. Meningitis is also more common in patients with multiple myeloma as compared to the average.
- Weakness and anemia: Weakness is one of the most common symptoms in multiple myeloma. It is usually due to anemia (a reduction in the number of red blood cells or hemoglobin levels).
In the physical exam, doctors may also find the following signs:
- Bony tenderness: It is ubiquitous, even in patients without a pathologic fracture.
- Liver and spleen swelling: It is also prevalent, known as hepatosplenomegaly. In some patients, there’s also deposition of immunoglobulin in the heart, resulting in cardiomegaly (an increase in the heart size).
- Signs of amyloidosis: There’s a deposition of amyloid plaques in different parts of the body. The most important signs include macroglossia (an increase in the size of the tongue), nodular skin lesions where amyloid is deposited, and swelling of the shoulder joints on both sides.
Stages and types of multiple myeloma
As noted above, patients typically undergo different stages before turning into multiple myeloma. The natural history of the disease usually goes like this:
- Monoclonal gammopathy of undetermined significance: It is the most common starting condition that leads to multiple myeloma. In this ailment, there’s a protein in the blood called M protein, which is synthesized in the bone marrow. In this ailment, there’s a base genetic alteration that overlaps with others and ultimately leads to multiple myeloma.
- Smoldering multiple myeloma: It is the precursor stage of multiple myeloma when plasma cells are already affected by several genetic alterations. In this stage, patients start displaying spinal lesions and may also have ongoing tumors found in an MRI scan, but patients are usually asymptomatic.
- Asymptomatic multiple myeloma: This is also known as stage 1 multiple myeloma. In this phase, there are not many cancerous cells, and patients remain asymptomatic. In some cases, they would have anemia and some weakness and may sometimes display bone damage and other lesions.
- Symptomatic multiple myeloma: Multiple myeloma usually start displaying symptoms in the second stage of the disease. In this phase, anemia is worse and usually causes severe weakness. Calcium levels in the blood are typically raised, causing some of the symptoms listed above.
- Comorbidities and complications: In stage 3, multiple myeloma causes severe anemia, a considerable loss of proteins eliminated in the urine, severe bone damage in at least three areas of the body, and rising calcium levels in the blood.
Diagnosis and tests
The diagnosis of multiple myeloma is very complex and combines different findings and tests:
- An assessment of monoclonal protein levels in the blood and the urine
- Magnetic resonance imaging
- Standard metaphase cytogenetics
- A biopsy or aspiration of the bone marrow
- Levels of lactate dehydrogenase, albumin, and beta-2 microglobulin
- Skeletal survey for pathologic fractures and other lesions
- Fluorescent in-situ hybridization
After performing all of these tests, or at least those appropriate for the patient, we need to join the results in two groups of diagnostic criteria and then join them in different combinations to determine whether or not the patient is to be diagnosed with multiple myeloma. It is a complex disease and a convoluted diagnosis, but it is easier for patients to understand the diagnostic tests and why are they used in each case:
- Blood studies: In many cases, the first sign of multiple myeloma comes from a blood test performed as a screening method or to rule out another disease. The patient usually has a reduction of one or more cell lines (anemia, leukopenia, or thrombocytopenia). In some cases, all cell lines are affected (pancytopenia). Protein levels in the blood are usually reduced, and uric acid can be increased. It is also recommended to use more advanced methods known as cell fluorescence in situ hybridization and serum-free light chain assay. They are useful to detect particular abnormalities found in multiple myeloma.
- Urine studies: Doctors usually ask for a 24-hour urine collection to measure creatinine clearance and other proteins in the urine. This is a reliable way to assess kidney function in this patient and define how bad is renal involvement in the disease. Another study that helps to detect kidney involvement is beta-2 microglobulin in the blood. Electrophoresis and immunofixation can also help doctors detect the type of proteins found in the urine.
- Radiography and other imaging studies: It is always a useful tool to rule out bone lesions and detect pathological fractures. In these patients, a complete skeletal series is recommended with an emphasis on the upper extremities. MRI can also be used to detect spinal cord compression and other spinal abnormalities.
- Bone marrow aspiration and biopsy: They are essential to detect the number of plasma cells in the bone marrow and their proliferation levels. They run histological and cytogenetic analyses to evaluate the morphologic and genetic differences in the bone marrow.
Treatment options
There is not a single treatment for multiple myeloma. Instead, the treatment protocol should be aimed at particular problems of each patient and their complications. There is no absolute cure for multiple myeloma. Still, several treatments are useful to reduce the burden of the disease, including thalidomide, lenalidomide, and dexamethasone in smoldering multiple myeloma, and different chemotherapy agents for multiple myeloma.
In some cases, multiple myeloma patients with severe disease are candidates for bone marrow transplantation. In this case, they should also receive immunosuppressant therapy to prevent rejection. Only advanced-stage disease with a high proliferative rate should be a candidate for a potential transplant. In these cases, elderly patients who have been recently diagnosed are not to be considered transplant candidates.
Other therapies include interferon alfa-2b, radiation therapy, bisphosphonate therapy for bone fracture prophylaxis, and adjunctive therapy with plasmapheresis, erythropoietin, corticosteroid, and many other agents according to each case.