Chronic Obstructive Pulmonary Disease, also known as COPD, is a respiratory disease that affects 32 million patients only in the United States. It ranks third as a cause of death and is a preventable cause of illness in many cases. There’s a classic triad in COPD that includes three different health problems: emphysema, chronic bronchitis, and asthma. COPD patients usually have a combination of two, and sometimes all three simultaneously.
Chronic bronchitis is a progressive respiratory problem featuring productive cough for a minimum of 3 months. Other causes of chronic cough are excluded, and the patient had these long cough episodes for at least two years.
Emphysema is another respiratory problem that develops over many years, usually due to chronic tobacco smoking. Emphysema features anatomic issues in the chest caused by an enlargement in the air spaces of the lungs. The walls of the airways are destroyed, and sometimes a fibrous tissue forms, similar to a scar.
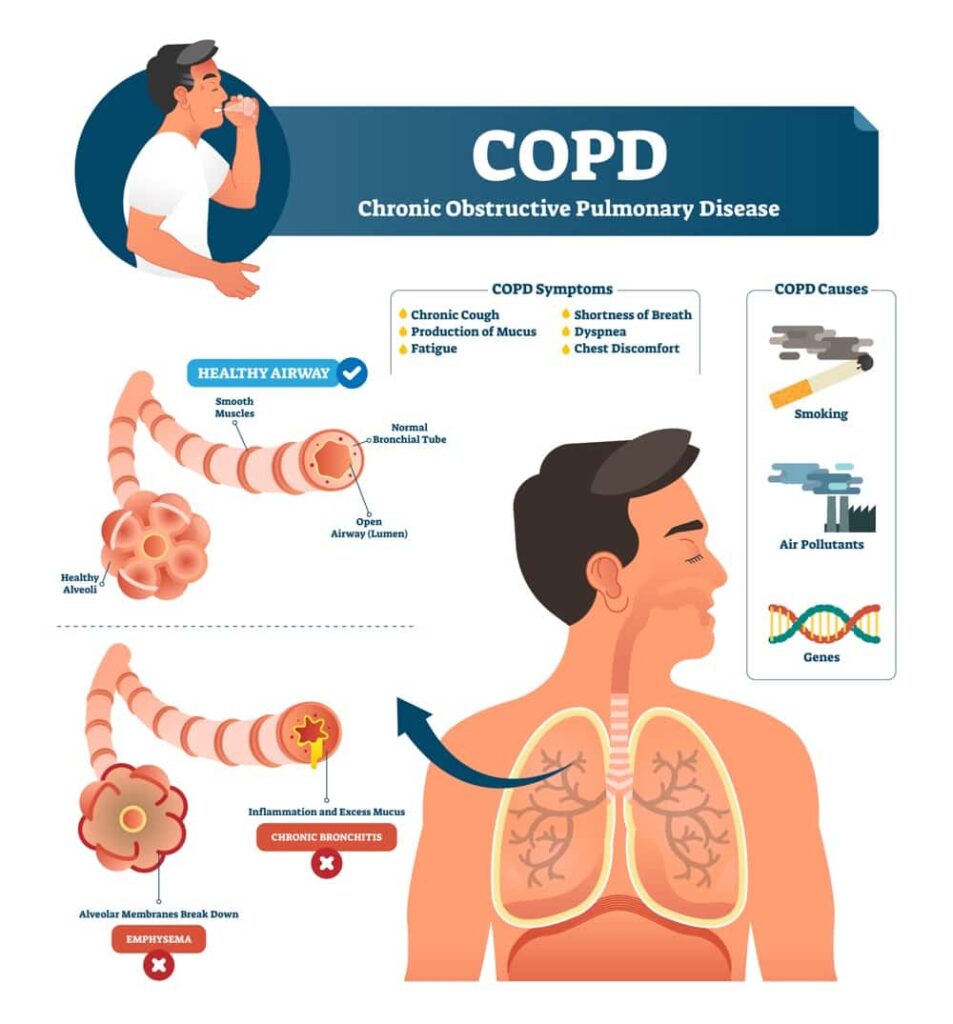
Asthma is an autoimmune problem combined with allergies. It causes inflammation in the airways and promotes changes in the walls. They become thick and start to secrete mucus.
Altogether, these entities are apparently different but have many things in common. Moreover, they often overlap in the same patient, and the severity of one triggers the other.
In this article, we will go through the most important signs and symptoms of chronic obstructive pulmonary disease (COPD). We will break them down into four groups. First, we will cover COPD symptoms in general and then specific signs and symptoms of COPD found in patients with chronic bronchitis, emphysema, and asthma.
COPD symptoms in general:
1. Progressive changes in symptoms
One of the challenges of diagnosing COPD is to detect the symptoms early in the course of the disease. In most cases, patients experience gradual symptoms that progress over many years. These patients usually minimize and ignore their symptoms and do not realize when they continue progressing. They will only realize something is wrong when the disease is severe and more difficult to treat.
2. Worsening dyspnea
One of the most critical symptoms of COPD is dyspnea. This is the clinical name for difficulty breathing that can be painful or simply distressing and uncomfortable. Patients often feel out of breath, and they often experience worsening symptoms in episodes. This type of breathlessness is progressive over the years and can be associated with wheezing sounds when the patient is breathing.
3. Chronic cough
This is also an important symptom in COPD, especially in patients with chronic bronchitis and asthma. In some patients, the incidence of cough may not be a relevant symptom, or it can be transient and without expectoration. Cough can be dry, but in most cases, it is productive, meaning it comes with mucus. Cough is maintained over the years without a clear cause, and it is typically worse in the early morning.
4. Wheezing on auscultation
Wheezing is a typical symptom of a patient with asthma, but other COPD patients may also have the same problem. In most cases, wheezing can be heard during auscultation. It is more evident during acute episodes but can sometimes be heard in other instances, depending on the severity of the disease.
4. Sputum production
This is a distinct feature of airway inflammation, and the symptom is present in almost every patient with COPD. They have ongoing inflammation that changes how the airway lining behaves. The glands in the airways secrete plenty of sputum to deal with debris and microorganisms, even when there is no reason to do it. Thus, patients continuously need to clear their airways, and their cough is usually productive.
5. Respiratory distress
In a late stage of the disease, patients may experience episodes of respiratory distress. In some cases, they may even faint due to a reduction of oxygen saturation in the blood. Patients with advanced COPD may start experiencing respiratory distress when they do simple house chores and other day-to-day activities. One of the giveaway signs is tachypnea or accelerated breathing, along with a sensation of running out of breath.
6. Cyanosis
This also happens in severe cases, especially in older adults with many years of COPD. Cyanosis is a change in the color of the skin and mucosa. The skin turns purple or adopts a blueish hue due to reduced oxygen in the blood. Cyanosis in COPD is more common in the distal portion of the hands and the patient’s feet.
7. Decreased breath sounds
Upon auscultation, doctors may also detect a reduction of breath sounds along with wheezing. They sound distant or reduced because there is not enough air going through the airways. This is due to airway wall modifications that reduce the available space for air to flow through.
8. Hyperresonance on percussion
Another physical exam maneuver is percussion, which is done by isolating an area of the chest and gently tapping between the ribs to hear the quality of the sound that is produced. In COPD patients, the sound is described as hyperresonance. It is a very particular sound that doctors can detect.
9. Prolonged expiration
People with COPD have more air inside the lungs than they can handle. Their inspiration volume decreases, and they tend to prolong their expiration volume. The respiratory cycle is the same in mild and moderate COPD, but the latter has more predominantly prolonged expiration. Inspiration, expiration, residual volume, and other measures can be taken by spirometry.
10. Coarse crackles in inspiration
You can also read about them as rales. It is a clicking or popping sound heard through the stethoscope. COPD patients are more likely to produce these sounds in inspiration, and it happens because air bubbles are formed as air passes through the fluid. It is a sign that the airways are filled with mucus. After coughing, the mucus dislodges, and the crackling sound reduces or goes away.
11. Reductions in fat mass
In COPD and after many years with the disease, patients start losing weight. The typical COPD patient has reduced fat mass, which does not make the patient look fit. It is more like a wasting syndrome, sometimes associated with cachexia, especially in emphysema patients.
12. Anemia
In COPD, anemia is one of the most likely comorbidities. Up to 33% of patients with COPD may develop anemia at some point. This is a type of anemia of chronic disease, caused by systemic inflammation. It contributes to the sensation of weakness or malaise as it further reduces oxygen availability.
13. Osteoporosis
Another systemic comorbidity of COPD is osteoporosis. It is basically a reduction of bone mineral density. This reduction in bone quality causes fragile bones and increases the propensity for fractures. It is more common in older adults, especially those with vitamin D deficiency and physical inactivity.
14. Changes in forced expiratory volume (FEV)
Expiratory volume is a spirometry measure useful to evaluate the severity of COPD. There are four stages of the disease. Patients are assigned to stage 1 or mild COPD when the FEV is 80% or more. Stage 2 or moderate COPD features FEV of 50 to 79%. Severe COPD has an FEV of 30 to 49%. And very severe COPD features an FEV lower than 30%.
15. Chronic bronchitis symptoms in COPD
Chronic bronchitis is not the same as Chronic Obstructive Pulmonary Disease. However, it is a part of the triad in COPD, and it is a common phenomenon in these patients. Chronic bronchitis in COPD increases the risk of airflow obstruction in patients with emphysema and predisposes them to respiratory infections. It features hypersecretion of mucus that obstructs the small airways, changes in the epithelium of the airways, and changes in airway surface tension.
The most important signs and symptoms include:
16. Comorbidity with obesity
This is not precisely a symptom. It is a comorbidity in chronic bronchitis or a related condition. But it is important because considering obesity helps doctors suspect chronic bronchitis in some patients. They are likely obese or overweight at the beginning of the disease. As the disease progresses and the condition becomes more severe, patients may start losing weight dramatically.
17. Cough with expectorations
One of the main features of chronic bronchitis is the formation of abundant mucus in the airways. COPD patients suffer from chronic cough, as mentioned above. Thus, chronic bronchitis in COPD has both cough and mucus. It is what doctors call productive cough, and it usually comes with clear mucus unless it is infected by bacterial agents.
18. Use of accessory muscles to breathe
In severe cases of chronic bronchitis, patients are more likely to experience severe symptoms of breathing difficulty. As they do, they may not even realize they are using extra respiratory muscles to assist their breathing. The use of accessory muscles is a common finding in the physical exam.
19. Coarse rhonchi on auscultation
These are also abnormal breathing noises and are different from the coarse crackles mentioned above. Rhonchi are low-pitched respiratory sounds that can be heard in inspiration or expiration and are often compared to a continuous snoring sound. Coarse rhonchi are produced when mucus clogs block the airway.
20. Signs of right heart failure
This only happens in severe chronic bronchitis and COPD cases. It causes pulmonary hypertension, cyanosis, and edema in the lungs. This is a response to low oxygen levels in the blood, which triggers an increase in lung blood pressure to make up for the deficit. But since the arteries are affected by COPD, they do not respond well to this adaptation.
21. Emphysema symptoms in COPD
Emphysema is so common in COPD that people usually confuse the terms and think COPD is the same as emphysema. However, it is only a part of the triad of COPD. Emphysema is the most common respiratory complication in smokers. Tobacco smoking for many years causes changes in the airways and the lung tissue enclosed in the spectrum of emphysema.
The most important signs and symptoms of emphysema in COPD include:
22. Impairments in systemic muscle function
Besides respiratory problems, there is usually a systemic muscle function problem in patients with emphysema. This is especially the case if the disease is caused by tobacco smoking. Muscle weakness and tiredness are likely symptoms of the disease.
23. A long history of progressive dyspnea
One of the top features of patients with emphysema is progressive dyspnea over the years. The disease does not have a sudden onset. Quite the opposite, and patients adapt to the changes and do not realize they are starting to run out of breath. This is also a feature of COPD but is more marked in the subset of emphysema patients.
24. Late onset of nonproductive cough
In patients with emphysema, they may not initially experience cough symptoms. At first, the leading symptoms are breathlessness and mucus production. The cough comes after a while, which is why we call it a late-onset symptom.
25. Cachexia
This is the name of a wasting syndrome found in different types of chronic diseases. It is often a bad sign and only happens when the condition is severe and difficult to treat. Cachexia features weight loss, muscle weakness, loss of appetite, and fatigue. It is a progressive symptom that affects the patient’s quality of life.
26. Barrel chest
This is an important sign in the physical exam and is characteristic of emphysema and COPD patients. We include this feature in emphysema symptoms because it is much more common in emphysema patients. Barrel chest is the classic name for an expansion of the diameter of the chest. It happens because the lungs are inflated with air caught in place and difficult to take out. So, the expiratory volume decreases, and there’s an excess of air in the lungs.
27. Distant heart sounds
This increase in the diameter of the chest is one of the reasons why the heart sounds are reduced when doctors use the stethoscope. They are often described as distant heart sounds. This does not necessarily mean that the heart has a problem, but sometimes we can have additional heart problems in patients with emphysema and COPD.
28. Respiratory failure
Along with cachexia, this is a late-onset manifestation of emphysema. As the disease becomes more severe, the respiratory compensation of increased accessory muscle use is insufficient to breathe normally. Patients experience frequent episodes of respiratory distress and may eventually have respiratory failure, which can cause mortality.
29. Assisted breathing and tripod sitting position
This is a symptom that patients are going through respiratory distress. The patient’s accessory breathing muscles are in use, and they lean forward when sitting down, resting the arms on the knees. This is unconscious, and some patients may avoid adopting this position if they know a doctor is expecting to see it.
30. Pulmonary hypertension
Not only do the airways and their walls change during COPD. There is also vascular remodeling in the lungs, which increases pulmonary artery pressure. This is a consequence of inflammation and hypoxia, which is more common in patients with severe emphysema due to capillary loss.
31. Asthma symptoms in COPD
Unlike emphysema, asthma is not mistaken for COPD because it is an integral part of the triad, but many patients with COPD do not have asthma. Also, most patients with asthma will never develop COPD. You can say asthma is an additional problem that worsens the signs and symptoms of COPD.
Patients with COPD and asthma will have the following additional signs and symptoms:
32. Audible wheezing without auscultation
One of the main features of asthma is wheezing, but COPD patients may also produce wheezing sounds. If they also have asthma, these sounds are more prominent, and it is more likely to hear them without auscultation. Wheezing sounds are produced when inflammatory changes significantly reduce the airway lumen in the wall and mucus.
33. Chest tightness
This is also a common sensation reported by patients with asthma. They feel tightness in the chest, similar to putting on very tight clothes. They feel difficulty taking a deep breath and may not only find it hard but also painful.
34. Sleep difficulty
Another essential feature of asthma is how it affects sleeping behaviors. Patients usually wake up several times at night with breathing difficulty and may develop insomnia and similar problems.
35. Reactive airway problems
Asthma is a reactive airway disease, which means that specific allergens trigger asthma symptoms. In response to these allergens, patients can experience a new disease flare-up. That’s why COPD patients with asthma experience an episodic worsening of the condition every time they come across allergens such as pollen, dust, mold, and tobacco smoke.
Conclusion
Chronic Obstructive Pulmonary Disease is a chronic respiratory condition that includes a triad of respiratory problems. They are chronic bronchitis, emphysema, and asthma. Patients may have two of these conditions or all three.
The most common signs and symptoms include breathlessness, mucus production, and chronic cough. However, every particular disease in the triad has its own characteristic signs and symptoms.
Treatment for COPD aims to improve the symptoms and reduce the exacerbations while preserving lung function as much as possible. These patients should consider smoking cessation to reduce mortality rates, and their follow-up is essential to prevent emergency situations with electrolyte alterations and other complications.